Have you ever woken up in the middle of the night with your mouth feeling like sandpaper? It’s not just uncomfortable—it can disrupt your sleep, make your teeth ache, and leave you worrying if something’s wrong. You’re not alone! Dry mouth at night, known medically as nocturnal xerostomia, is far more common than most people realize, especially as we get older. But understanding what triggers that sticky, parched sensation is the first step toward real relief.
In this detailed guide, you’ll learn about the 8 most common reasons for waking up with dry mouth and what you can do about each one. By the end, you’ll have practical prevention tips and know when it’s time to talk with your dentist or doctor.
Key Takeaways:
- Nighttime dry mouth has many causes, from natural changes with age to medications, mouth breathing, and serious health conditions.
- Some triggers are easy to fix at home, but persistent symptoms deserve medical attention.
- Protecting your saliva matters for your teeth, digestion, and sleep quality!
1. Natural Nighttime Saliva Changes and Aging
Did you know your body automatically reduces saliva production while you sleep? That’s completely normal—but if you’re over 60, studies show this nighttime reduction gets more noticeable. Researchers have found that unstimulated (resting) saliva drops by as much as 38–44% as we age. This is why older adults often notice a dry mouth, especially at night. But aging alone rarely causes severe dryness: it’s usually part of a bigger picture with other factors at play, such as medications or breathing habits. If you’re older and noticing more dryness, have a chat with your dentist; it’s common but shouldn’t be ignored.
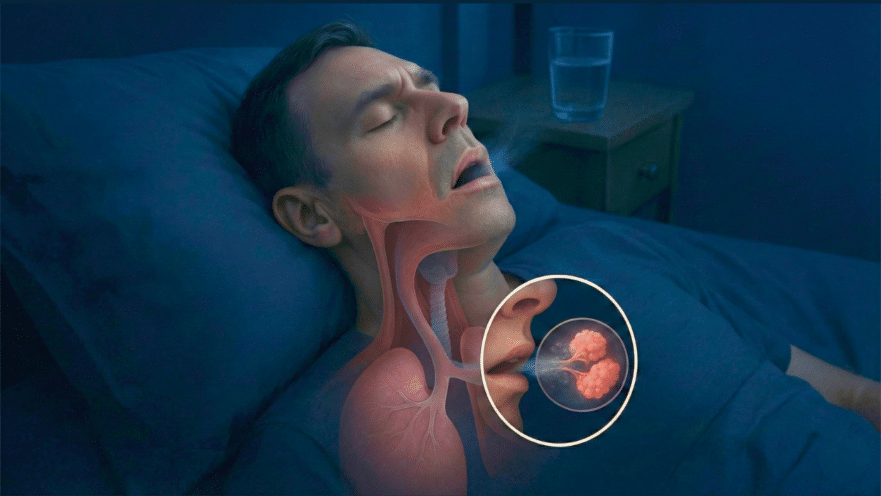
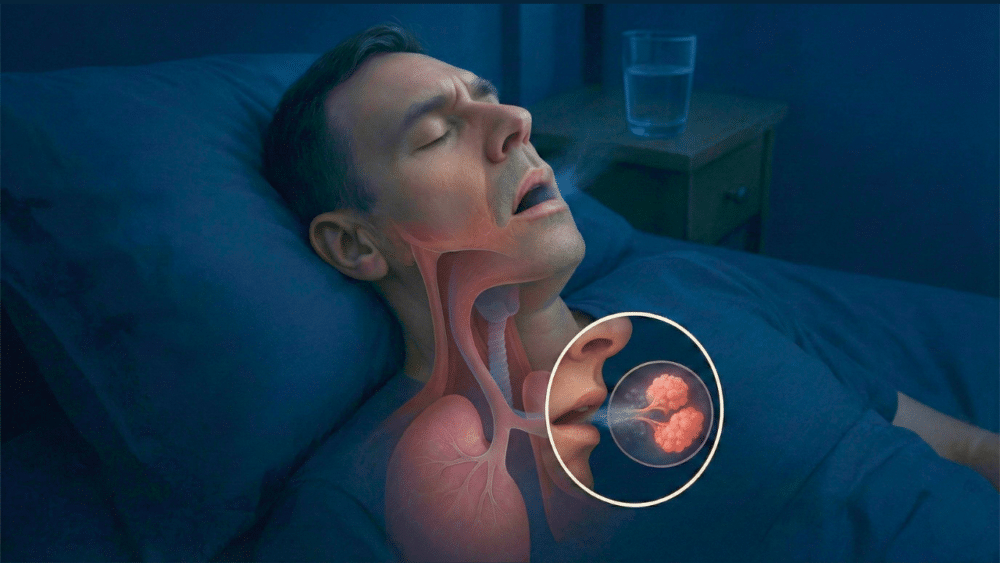
2. Mouth Breathing, Snoring, and Sleep Apnea
Breathing through your mouth instead of your nose, whether you realize it or not, can dry out your mouth rapidly overnight! Snoring and sleep apnea—where breathing stops and starts repeatedly—often force you to open your mouth to get more air. This exposes your delicate oral tissues to airflow, causing evaporation of saliva. If you wake up with a dry mouth alongside snoring, gasping, or fatigue, ask your doctor about possible sleep-disordered breathing. Solutions can include treating nasal congestion, using saline rinses, or if necessary, a CPAP machine or dental appliance to keep your airway open.
3. Medication Side Effects and Polypharmacy
Over 500 prescription and over-the-counter medicines have dry mouth as a side effect! The most common culprits include medications for allergies, high blood pressure, depression, pain, and bladder control. Many of these block nerve signals that keep saliva flowing. If your dry mouth started soon after starting a new medication, it’s worth discussing options with your doctor. Sometimes a dosage adjustment, a switch to another drug, or adding saliva-stimulating habits like chewing sugar-free gum or using a saliva substitute can provide relief. Never stop your medications on your own—always seek your healthcare provider’s guidance first.
4. Dehydration, Caffeine, Alcohol, and Evening Habits
Simple evening choices can dry out your mouth overnight more than you think. Not drinking enough water means your body makes less saliva. Caffeine and alcohol are both dehydrating and decrease saliva flow; alcohol even relaxes your throat muscles, which can worsen snoring and dry mouth. Tobacco further irritates the mouth and reduces saliva. To help, try sipping water throughout the evening, keep a glass of water by your bed, cut back on alcohol and caffeine at night, and avoid alcohol-based mouthwashes. Sugar-free lozenges or gum before bed can also boost saliva.
5. Autoimmune Diseases Such as Sjögren’s Syndrome
Sometimes, dry mouth at night can be a sign of an autoimmune disease. Sjögren’s syndrome causes the immune system to attack the moisture-producing glands, leading to severe, lingering dryness in the mouth and eyes. This triggers constant symptoms—often worse at night. Other signs to watch for are dry eyes, joint pain, fatigue, or swelling near the jaw. Getting an early diagnosis from a specialist is crucial: treatment might include sips of water, special saliva substitutes, and sometimes prescription medications that stimulate salivary glands.
6. Diabetes and Other Systemic Health Conditions
Chronic health conditions, especially diabetes, can quietly reduce saliva. High blood sugar changes blood vessels and nerves serving the mouth, increasing your risk of dehydration—even if you don’t notice at first. Neurological problems, yeast infections, or prior injuries to the head and neck can also interfere with saliva production. If you have diabetes or similar health challenges and begin to experience new, persistent dryness at night, let your care team know. Improving hydration, managing underlying conditions, and regular dental checkups can make a significant difference.
7. Smoking, Vaping, and Recreational Drug Use
It’s no secret: smoking and vaping leave your mouth dry. The heat, chemicals, and reduced blood flow from these habits damage salivary glands and raise your risk for gum disease and oral cancers. Many people notice their dry mouth improves after quitting tobacco or vaping. Additionally, recreational drugs such as stimulants, cannabis, and some painkillers can drastically suppress saliva for hours—especially disastrous if used at night. If you use these substances and are struggling with dryness, consider seeking help to quit, and ask your dental professional about protecting your teeth during recovery.
8. Cancer Treatments and Injury to Salivary Glands
If you’ve undergone radiation for head or neck cancer, certain chemotherapy regimens, or had surgery removing part of your salivary glands, you may face lasting, even permanent, dry mouth—especially at night. Damaged glands often can’t recover completely. These cases require dedicated strategies: prescription medications to stimulate saliva, fluoride treatments, custom trays, and sometimes special gels or humidifiers to get through the night comfortably. Keeping in close contact with your dental team is absolutely vital to prevent infection and tooth decay.
How to Prevent Dry Mouth at Night—and When to Seek Help
Most cases of nighttime dry mouth respond well to simple lifestyle and habit changes. Here are some tips:
- Chew sugar-free gum or suck on sugar-free candy to stimulate saliva flow.
- Sip water throughout the evening and keep some by your bedside.
- Breathe through your nose by treating nasal congestion before sleep.
- Limit alcohol, caffeine, and tobacco use in the hours before bed.
- Visit your dentist regularly, and use fluoride toothpaste to protect your teeth.
If your dryness persists, is severe, or you notice other symptoms like trouble swallowing, gritty eyes, swollen glands, or unexpected dental problems, don’t wait—see your dentist or doctor. Persistent dry mouth can lead to serious oral health problems if left untreated. Early intervention protects your smile and your well-being!