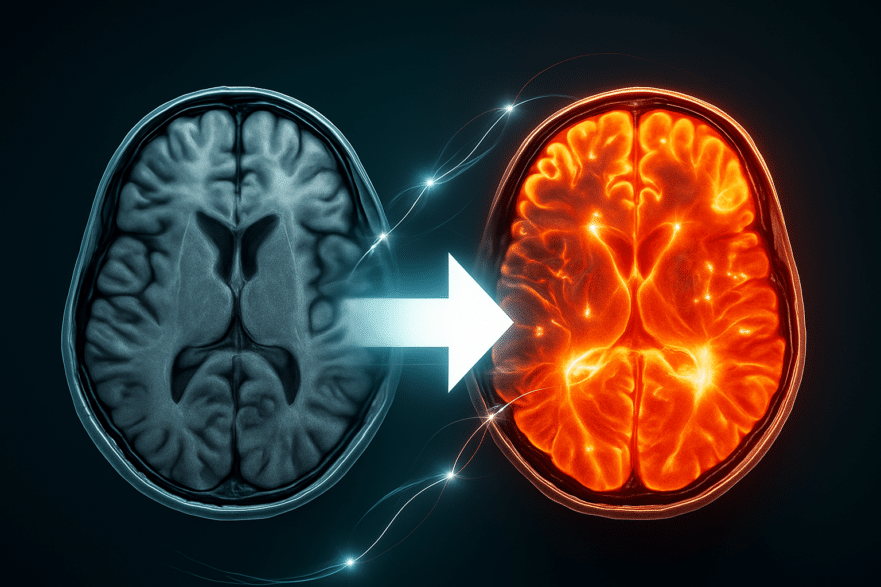
Have you ever worried that the very medications meant to protect your heart might be harming your brain? It’s a common concern, especially with all the conflicting information out there about cholesterol. Your brain is packed with it—holding about 20% of your body’s entire supply—and it’s absolutely critical for your nerve cells to communicate. So, it’s natural to wonder: if you lower your blood cholesterol, are you accidentally starving your brain of a vital nutrient? A groundbreaking new study of over one million people is helping to clear up this controversy, and the findings are too important to ignore. This research gives us fresh, powerful data on what’s really going on with cholesterol, brain health, and dementia risk.
In this article, we’re going to dive deep into this fascinating topic. We’ll unravel the complex relationship between cholesterol and your brain, look at what the science says about cholesterol-lowering medications like statins, and, most importantly, give you practical, actionable steps you can take—starting today—to protect your cognitive health for the long haul. This isn’t just about cholesterol; it’s about a holistic approach to building a dementia-resistant brain. (Based in the insights of Dr. Brad Stanfield)
Key Takeaways
- Your Brain Makes Its Own Cholesterol: The cholesterol in your brain is made by your brain. Lowering your blood cholesterol through diet won’t harm it, but the role of medications has been a subject of debate.
- Long-Term Statin Use Appears Highly Protective: While short-term clinical trials have shown mixed results, long-term observational studies and new genetic research suggest that using statins for years can slash dementia risk significantly.
- Midlife Health is Crucial: The evidence strongly indicates that managing cholesterol levels in your 40s and 50s has a powerful protective effect against developing dementia later in life. It’s a long-term investment in your future brain.
- Dementia Prevention is More Than Just Cholesterol: Key modifiable risk factors include managing blood pressure, preventing type 2 diabetes, staying active, and addressing four often-overlooked areas: cognitive stimulation, hearing loss, vision impairment, and depression.
1. The Cholesterol Conundrum: Friend or Foe to Your Brain?
Let’s start by addressing that big worry head-on. Could lowering your blood cholesterol actually be bad for your brain? It’s a valid question. After all, cholesterol is a building block for the very structures that allow your neurons to fire and communicate. Without it, your brain simply can’t function properly. So, if you actively lower your cholesterol levels, are you putting your brain at risk?
The answer, it turns out, depends on how you lower it. Here’s a fascinating fact: cholesterol doesn’t cross the blood-brain barrier. This protective shield keeps your brain’s environment stable. This means the cholesterol in your brain isn’t supplied from the food you eat or what’s circulating in your blood; it’s manufactured right there, on-site, by specialized brain cells. So, if you lower your blood cholesterol through diet and lifestyle changes, you don’t have to worry about depriving your brain. The two systems are separate.
2. Statins and Your Brain: Unraveling the Controversy
The story gets a bit more complicated when we talk about cholesterol-lowering medications like statins. Some evidence from lab and animal studies suggests that certain statins can cross the blood-brain barrier, which in theory could lower the brain’s own cholesterol production. Early on, some doctors reported cases where patients on statins experienced memory loss, which often improved when they stopped the medication. This created a lot of concern.
However, when we look at higher-quality evidence from large, randomized controlled trials, the picture changes. The Prosper study, for example, followed elderly participants for over three years and found no difference in cognitive decline between those taking a statin and those taking a placebo. A more recent study that followed patients for five years—who achieved very low LDL levels using a combination of statins and another powerful drug class called PCSK9 inhibitors—also found no negative cognitive effects. The evidence we have so far strongly suggests that these medications do not harm your cognitive health.
3. Can Lowering Cholesterol Actually Prevent Dementia?
If statins don’t harm the brain, could they actually help it? This is where things get really interesting. Observational studies, which look at large populations over many years, have consistently pointed to a link between statin use and a lower risk of dementia. A massive meta-analysis combining 55 studies and over 7 million patients found that statins cut the risk of dementia by 14%. Even more impressively, for those who used statins for more than three years, the risk reduction was a staggering 63%.
To understand why, it helps to know that there are two main types of dementia. Vascular dementia is caused by plaque buildup in the arteries that supply blood to the brain, starving brain cells of oxygen. Alzheimer’s disease involves damage to brain cells from the accumulation of broken proteins. High LDL, or “bad” cholesterol, is a primary cause of the plaque that contributes to both conditions. By lowering LDL, statins directly combat this plaque buildup. They also have powerful anti-inflammatory and antioxidant effects, which can further protect brain cells from damage.
4. Why Clinical Trials Tell a Different Story (And What It Means for You)
Here’s the puzzle: if observational studies show such a strong protective effect, why haven’t randomized controlled trials (the gold standard of medical research) found the same thing? A recent meta-analysis of 20 trials with over 100,000 participants found that lowering LDL with medication did not lower dementia risk within the timeframe of the studies.
One possible explanation is something called “healthy user bias”—people who take preventative medications like statins are often more likely to engage in other healthy behaviors, like exercising and eating well. But a more compelling reason is time. Research shows that your LDL cholesterol levels in midlife are strongly linked to your risk of developing dementia decades later. This suggests that to protect your brain, you need to manage cholesterol over a very long period. Most clinical trials only last a few years, which may not be long enough to see the brain-protective benefits that take decades to appear.
5. The Breakthrough: What a 1-Million-Person “Lifetime Trial” Revealed
This is why the new study is so important. Researchers used a clever method called Mendelian randomization. Instead of giving people a drug for a few years, they studied people who were born with natural genetic variations that mimic the effect of cholesterol-lowering drugs. It’s like they’ve been on a statin their entire life, without ever missing a dose. By comparing them to people without these genes, scientists can see the true lifetime effects of lower cholesterol.
The results were astounding. People with a gene variant that simulated the effects of statins had a 76% lower risk of dementia. Those with a variant mimicking another drug, ezetimibe, had an 82% risk reduction. This provides powerful support for the idea that long-term, lifelong management of LDL cholesterol is highly protective against dementia. It helps us see what the short-term clinical trials are missing.
6. Beyond Cholesterol: 4 Hidden Dementia Risk Factors You Can Control
Managing your cholesterol is a huge step, but it’s just one piece of the puzzle. The Lancet Standing Commission has identified several other key modifiable risk factors. While things like inactivity, type 2 diabetes, high blood pressure, and obesity are well-known culprits, here are four hidden risk factors you might be overlooking:
- Lack of Cognitive Stimulation: Just like your muscles, your brain thrives on being used. A study of over 100,000 people found that those with mentally stimulating jobs had a lower risk of dementia. The takeaway is simple: keep learning, stay curious, and challenge your mind. It’s one of the best things you can do for your long-term brain health.
- Untreated Hearing Loss: When your ears don’t transmit clear signals, your brain isn’t getting the stimulation it needs and can begin to weaken. Research shows a clear link between untreated hearing loss and up to a 2.4 times higher risk of dementia. The good news? A systematic review found that using hearing aids significantly lowers this risk. If you’re struggling to hear, get it checked.
- Poor Vision: The same principle applies to your eyes. If your vision is poor, the signals reaching your brain are weak. A major meta-analysis of over 6 million adults found that those with vision loss had a 47% higher risk of developing dementia. Taking your vision seriously and getting it corrected is another critical piece of protecting your brain.
- Depression & Social Isolation: Your mental and social well-being are deeply connected to your brain health. Studies show that people with depression, especially in midlife, have more than double the risk of developing dementia later on. Thankfully, treating depression with therapy or medication can reduce this risk by about 30%. Similarly, social isolation is a known risk factor, so prioritizing your connections with others is essential.
7. Promising Supplements for Brain Health
Once you have the main lifestyle factors under control, a few supplements have shown some promising evidence for supporting brain health. A large trial found that taking a daily multivitamin and mineral supplement led to improvements in cognition and memory equivalent to reducing brain aging by two years.
Creatine, long known for boosting muscle performance, also plays a vital role in energy production in the brain. A 2022 meta-analysis showed that creatine supplements improved memory, especially in older adults. Finally, TMG (trimethylglycine) may help by lowering levels of an amino acid called homocysteine. High homocysteine is strongly linked to Alzheimer’s disease, and TMG is effective at reducing it. While this isn’t a guaranteed way to prevent Alzheimer’s, it’s a promising area of research. As always, you should speak with your doctor before starting any new supplement regimen.
Conclusion
The evidence is becoming clearer every day: protecting your brain from dementia is a long-term game, and the choices you make in midlife have a profound impact decades down the road. The debate over cholesterol is settling, with compelling new research showing that managing your LDL cholesterol over the long haul is a cornerstone of dementia prevention. But it doesn’t stop there. By embracing a holistic approach—challenging your mind, staying socially connected, taking care of your hearing and vision, managing your mental health, and adopting a healthy diet and exercise routine—you are building a more resilient, healthier brain. You have the power to take control of your cognitive future, and the time to start is now.
Source: Dr. Brad Stanfield