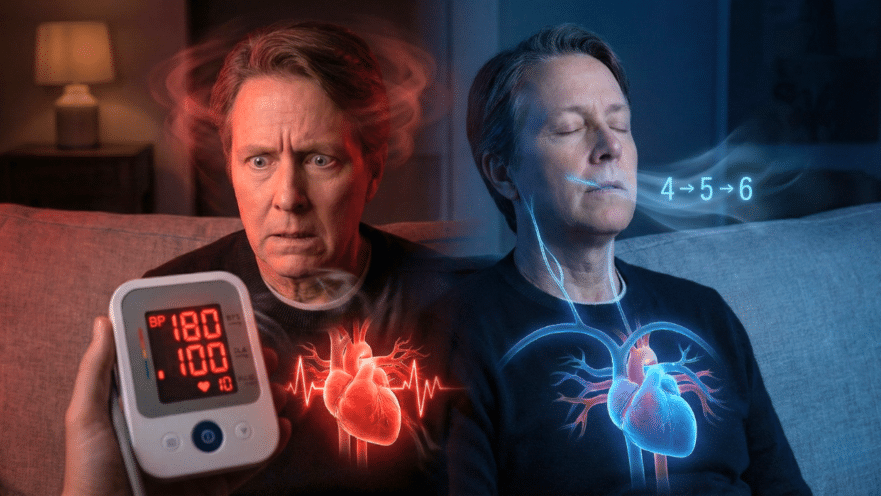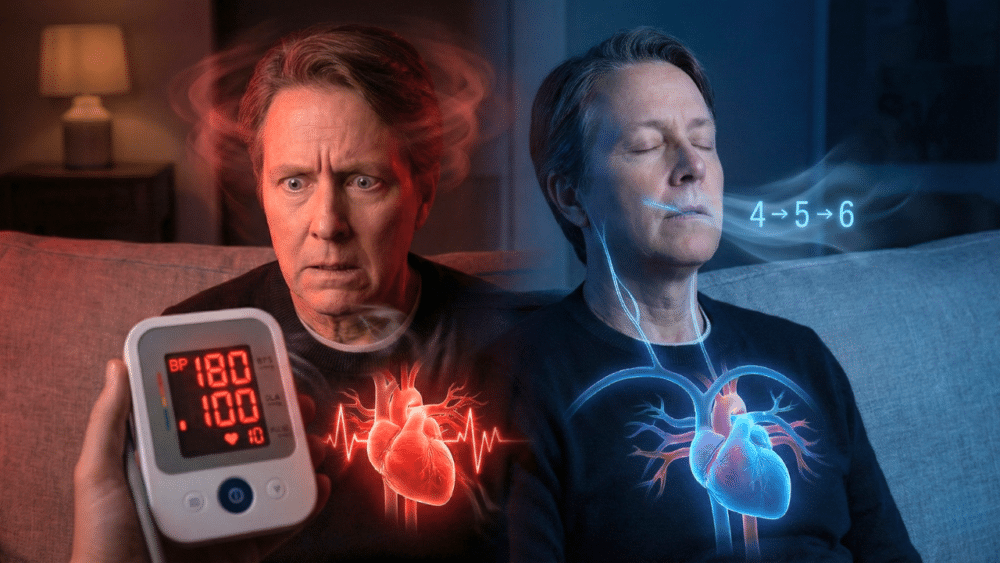
Ever found yourself checking your blood pressure at home, only to see a number like 180 over 100? You might instantly panic, feeling your heart race, your hands get sweaty, and ask yourself: “Is this a heart attack? Am I having a stroke? Should I rush to the ER?” Before you grab your keys and head to the hospital, hold on just a second. Understanding what these numbers actually mean—and what you should do next—can make all the difference to your health.
Today, I’m going to walk you through the truth behind high blood pressure spikes, when to worry, what really works to bring your pressure down quickly, and why those old-school emergency pills might be more dangerous than helpful. Let’s clear the confusion and equip you with the keys to manage this situation calmly and safely. (Based on the insights of cardiologist, Dr. Juan Veller)
Key Takeaways:
- High blood pressure readings at home, even as high as 180, are rarely an emergency on their own.
- Taking medication or doubling up on pills without medical supervision can be risky.
- There are practical, proven strategies you can use at home to safely calm yourself and reduce your BP.
- Knowing the warning signs of a true emergency is critical—and I’ll teach you how to spot them.
1. Don’t Panic: High Numbers Alone Aren’t Always Emergencies
It’s natural to be alarmed when your blood pressure monitor flashes 180/100, but take a deep breath. Most of the time, a single high reading is not a medical emergency, especially if you don’t have any other symptoms. Cardiologists today know that treating just the number—without considering symptoms and the bigger picture—isn’t always the best approach.
2. Ask Yourself Two Crucial Questions
Before doing anything, check in with yourself:
- Do you feel any pain, in your head, chest, or back?
- Did something emotional just happen to you in the last couple of hours?
Arguments, stressful events, or celebrations can send your numbers soaring temporarily. If you’re feeling okay or have only a mild headache, most experts agree you don’t need to rush to the ER.
3. Avoid Self-Medicating with Rapid-Acting Pills
Dr. Google or well-meaning relatives might tell you to take a “sublingual pill” or double up on your meds, but this is outdated—and risky. Rapidly lowering your blood pressure with medication you haven’t been prescribed (or more than your prescribed dose) can be dangerous. Your brain and organs may have gotten used to higher pressures and a sudden drop can cause serious complications.
4. Stop the Cycle: Don’t Obsessively Check Your BP
It’s easy to get stuck in a loop—see a high number, get stressed, check again, number goes up, stress climbs, and on and on. Don’t fall into this trap! Checking your BP every couple of minutes increases anxiety and can keep your pressure high.
5. Try These Proven Calming Techniques
A. Real Rest:
- Turn off the TV, music, and even dim the lights.
- Find a comfortable spot, maybe lie down, and read something calming.
- Avoid stressful conversations or sensational news.
B. Simple Pain Relief:
- If you have a mild headache or backache, a common over-the-counter painkiller like acetaminophen (paracetamol) can help—but don’t overuse it.
- Sometimes just a glass of water can help if you’re dehydrated.
C. The 4-5-6 Breathing Technique:
This trick activates your body’s “brake system” (the parasympathetic nervous system), which helps slow your heart rate and lower pressure.
- Inhale calmly for 4 seconds.
- Hold your breath for 5 seconds.
- Exhale slowly for 6 seconds.
- Repeat for 2-3 minutes in a quiet setting.
Count it out and focus on your breath. You’d be surprised how much this simple method helps.
6. Know When It Is an Emergency: Red Flag Symptoms
Most isolated high BP readings aren’t emergencies—unless… you experience symptoms indicating an organ is in trouble. Seek ER help immediately if your high BP comes with:
- Chest pain: Pressure, burning, or an intense discomfort different from any usual indigestion.
- Shortness of breath: Fast breathing, unable to catch your breath.
- Neurological symptoms: Slurred speech, drooping of the face, weakness in an arm or leg, blurred vision, confusion, or inability to move a limb.
- The worst headache of your life: Not your routine post-work headache, but a severe, sudden headache you’d rate as unbearable.
These could signal a stroke, heart attack, or other dangerous condition. Don’t wait around—call emergency services or go straight to the ER.
7. Be Smart: Track Your BP and Follow Up
If you feel fine and the spike seems linked to an emotional event or stress, try the calming steps above. Once you’ve settled, jot down your BP numbers each morning for a couple of weeks. Don’t stress if your doctor’s appointment is a week or two away—you’re giving your doctor valuable information for a better diagnosis and plan.
If you’re already being treated for high blood pressure, keep taking your medication as prescribed, eat less salt, exercise regularly, and avoid obsessing over every reading. Your pressure will naturally vary with the ups and downs of daily life and that’s normal.
Remember:
- Cardiologists treat people, not numbers! A single high reading usually isn’t dangerous. What matters most is how you feel and whether there are symptoms of organ damage.
- Routine, organized tracking and staying calm will do you more good than panic and rushed decisions.
**Feeling scared is natural, but knowledge is powerful. The next time your pressure spikes, remember this guide. And if anything isn’t clear, talk to your doctor, or leave your questions and experiences for us! Stay safe and take care—you’ve got this!
Source: Dr. Juan Veller