What if I told you that the “perfect” blood pressure number you’ve been told to chase—120 over 80—could actually be doing you more harm than good? It sounds counterintuitive, I know. We’ve had it drilled into our heads that this is the gold standard for cardiovascular health. But the truth is, medicine is not one-size-fits-all, and your body is unique. The rigid pursuit of a single number for every single person, regardless of age or individual health status, is a deeply flawed approach that can lead to dangerous consequences. It’s time we had an open, honest discussion about what a healthy blood pressure really looks like for you.
This isn’t about ignoring the risks of truly high blood pressure. It’s about questioning the aggressive, number-chasing mentality that has taken over modern medicine. We’re going to dive into why your ideal blood pressure might be different from the textbook standard, the hidden dangers of over-treatment, and most importantly, how you can take back control of your health by understanding your own body and advocating for personalized care. (Based on the insights of Dr. Suneel Dhand)
Key Takeaways
- The “120/80” Goal is Not Universal: This standard number is not appropriate for every individual, especially as you get older.
- Over-Treatment is Dangerous: Forcing blood pressure too low can cause dizziness, brain fog, falls, and even damage to your brain and kidneys from poor blood flow.
- Your Ideal Blood Pressure Changes with Age: As arteries naturally stiffen over time, a slightly higher blood pressure may be necessary to ensure your organs get enough blood.
- Accurate Home Monitoring is Your Best Tool: Learning how to properly measure your blood pressure at home gives you and your doctor the real data needed to make smart decisions.
- Lifestyle is the Foundation: The most powerful way to manage blood pressure is by addressing the root cause, which is often related to diet, stress, sleep, and exercise.
- You Must Be Your Own Advocate: It’s crucial to have open conversations with your doctor and question whether your current medication plan is still right for you.
1. What Do Your Blood Pressure Numbers Actually Mean?
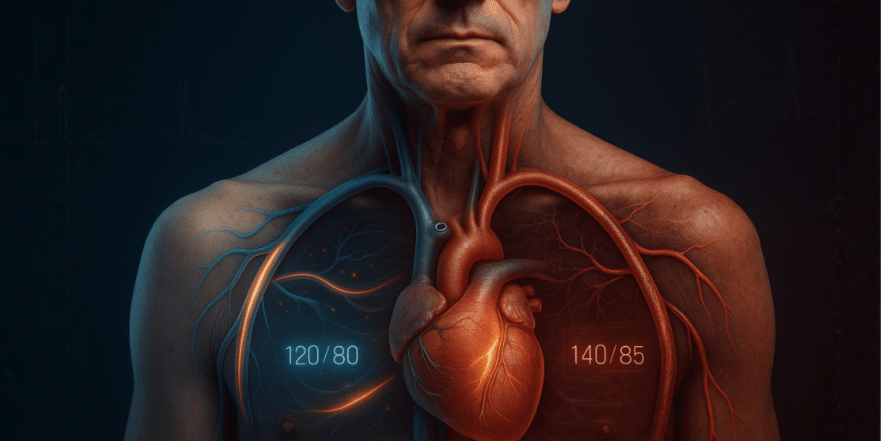
Before we can challenge the numbers, you need to understand what they represent. When you get a blood pressure reading, you see two numbers, like 120/80 mmHg. Here’s the simple breakdown:
- The Top Number (Systolic): This is the pressure in your arteries when your heart muscle contracts or squeezes to pump blood out to the rest of your body. Because the heart is actively pushing, this is the higher of the two numbers.
- The Bottom Number (Diastolic): This is the pressure in your arteries when your heart muscle is relaxed between beats. Since the heart is resting and filling with blood, the pressure is lower.
While doctors look at both numbers, there’s often more focus on the top (systolic) number. In most cases, if one number is high, the other tends to be high as well. Understanding this basic mechanism is the first step to grasping why simply forcing these numbers down isn’t always the answer.
2. The Problem with “Guideline Rigidity”: Chasing Numbers, Not Health
The medical establishment loves guidelines. They provide a simple framework for treating common conditions. However, when these guidelines become rigid rules, we start treating the numbers on a chart instead of the actual person sitting in front of us. The idea that every adult, from a 25-year-old athlete to an 85-year-old retiree, should aim for the exact same blood pressure is, frankly, a bit crazy.
Your body is a complex, dynamic system. What is a healthy blood pressure for one person can be dangerously low for another. This obsession with hitting a target of 120/80 often leads to aggressive medication, without considering the patient’s overall well-being, symptoms, or quality of life. It ignores the simple fact that we are all different.
3. The Hidden Dangers of Low Blood Pressure
We’re constantly warned about high blood pressure, but what about blood pressure that’s too low? This is a massive, under-recognized problem, especially in older adults who have been over-medicated. When your blood pressure is pushed too low, your vital organs don’t get the blood flow—and therefore oxygen and nutrients—they need to function properly. This is called under-perfusion, and it can be incredibly harmful.
Symptoms of overly low blood pressure include:
- Dizziness, lightheadedness, or feeling faint
- Brain fog and memory issues
- Chronic fatigue and weakness
- Increased risk of falls, which can lead to fractures and a rapid decline in health
Your brain and your kidneys are particularly vulnerable. Reduced blood flow to the brain can cause cognitive symptoms that are often mistaken for normal aging. Meanwhile, your kidneys, which naturally lose function over time, can suffer accelerated damage when they aren’t adequately perfused. The very treatment meant to protect you can end up causing a different, more immediate set of problems.
4. Why Your Age Matters: The Case for Higher Blood Pressure in Older Adults
As you age, your major arteries naturally become stiffer and less flexible, a process known as arteriosclerosis. Think of it like trying to push water through a rigid pipe versus a flexible hose. To get blood to all your vital organs through these stiffer vessels, your body may need to generate a bit more pressure.
In this context, a systolic blood pressure of 140 or even 150 might be your body’s natural, healthy adaptation. Forcing it down to 115 with medication could leave you feeling dizzy and weak because your brain isn’t getting the circulation it needs. Some research has even shown a U-shaped curve for mortality in the very elderly (over 85), where those with systolic pressures in the 150s actually had better outcomes than those with very low or very high pressures. While this doesn’t mean 150 should be everyone’s new goal, it powerfully illustrates that the “lower is always better” mantra is dangerously oversimplified.
5. The Scandal of Over-Medication: A Story You Need to Hear
This isn’t just a theoretical problem; it’s happening to millions of people. Consider this true story: a man in his late 70s, who was put on blood pressure medication in his 40s. Over the decades, as is common, more doctors added more pills. He started feeling dizzy, unwell, and just “not himself.” One morning, after making breakfast, he felt extremely faint. His blood pressure was checked, and the top number was in the 70s—a dangerously low reading. He was pale and on the verge of collapse.
Looking back, it was clear he had been over-medicated for a long time. His body had changed, perhaps his health had improved, but his prescriptions hadn’t. After stopping one medication and drastically reducing another, he began to feel like himself again. This story is a classic example of polypharmacy, where medications are piled on but rarely re-evaluated or stopped. It’s a scandal of epic proportions, driven by a system focused on medicating numbers.
6. How to Take Back Control: Master Home Blood Pressure Monitoring
If you are on blood pressure medication, the single most empowering thing you can do is monitor your numbers accurately at home. This gives you the real-world data you need to have an intelligent conversation with your doctor. Don’t rely solely on the one-off reading at the clinic.
Here’s how to do it right:
- Get the Right Cuff: Use an automatic, upper-arm cuff. Brands like Omron are generally reliable. Wrist cuffs are often less accurate.
- Prepare Properly: Before you take a reading, sit quietly in a comfortable chair for at least 5 minutes. Don’t drink caffeine, exercise, or smoke for 30 minutes beforehand. Your arm should be supported at the level of your heart.
- Measure Consistently: Check your blood pressure in the morning before you take your medications, and again in the evening. Take three separate readings, a minute or two apart, and average them. This gives you a much more stable and accurate picture than a single measurement.
- Keep a Log: Do this for two weeks and write down all the readings. Bring this log and your machine to your next doctor’s appointment. You can even check your machine’s accuracy by comparing its reading to the one taken in the office.
7. Don’t Be Fooled by “White Coat Hypertension” (But Understand It)
“White coat hypertension” is a real phenomenon where your blood pressure is high in a medical setting but normal at home. The stress of a doctor’s visit—fighting traffic, waiting, anxiety about the appointment—can temporarily spike your readings. This is precisely why home monitoring is so vital.
However, don’t let it become a blanket excuse to ignore high readings. It’s important to confirm that your pressure is truly normal at home. A great tip is to ask your doctor or nurse to re-check your blood pressure at the end of your visit, after you’ve had a chance to sit and talk, which often shows a significantly lower reading.
8. The Ultimate Solution: Reversing High Blood Pressure Naturally
For a vast number of people, especially those who develop high blood pressure at a younger age, the root cause is not a medication deficiency. It’s a lifestyle issue, most commonly insulin resistance. When your body is resistant to the hormone insulin (often due to a diet high in sugar and processed carbs), it can lead to high blood pressure through several mechanisms, including causing your kidneys to retain sodium and making your arteries stiffer.
The good news is that this is reversible. The pillars of good health are your most powerful medicine:
- Diet: Focus on whole, unprocessed foods.
- Exercise: Find an activity you love and aim for 20-30 minutes a day.
- Stress Management: Chronic stress keeps your body in a high-alert state, raising blood pressure.
- Quality Sleep: Poor sleep is a major stressor on the body and directly impacts blood pressure.
By addressing these areas, you can often improve your metabolic health so dramatically that your blood pressure normalizes, allowing you to reduce or even eliminate your need for medication, with your doctor’s guidance.
Conclusion: You Are Unique, and Your Health Should Be Personal
It’s time to move away from the industrialized, one-size-fits-all model of medicine and return to a personalized approach. You know your body better than anyone. If your blood pressure numbers look “perfect” on paper but you feel terrible, then that is not the right blood pressure for you. The goal should be to live your healthiest, most vibrant life, not to chase a number in a textbook. Be active, eat well, manage stress, and most importantly, partner with a doctor who listens to you and treats you as the unique individual you are. Don’t be afraid to ask questions and advocate for a plan that makes you feel good, not just one that satisfies a guideline.
Source: Dr. Suneel Dhand