If you’re taking medicine for diabetes, high blood pressure, cholesterol, pain, or even heartburn, you might be surprised to learn that some of these may be putting your kidneys at risk. It’s not just about watching your sugar and blood pressure. Some commonly used drugs can gradually wear down your kidneys, sometimes without any clear warning signs until trouble appears. The good news? Much of this damage can be caught early—or even reversed—if you know what to look for.
As a health educator, I’m here to walk you through the seven most common nephrotoxic (kidney-harming) medications that may be sitting in your medicine cabinet. Understanding these can help you have informed conversations with your healthcare provider and better protect your kidney health. (Based on the insights of Dr. Antonio Cota)
Key Takeaways:
- Your kidneys are essential for overall health.
- Some common medications can quietly harm your kidneys over time.
- Knowing which medications to watch for, and regular check-ups, can help protect your kidney function.
- Always talk to your doctor before stopping or switching any prescribed drugs.
1. Aminoglycoside Antibiotics (Amikacin and Similar Drugs)
These antibiotics—like amikacin—are often prescribed by injection to treat serious infections. Today, their use is a bit less common, but they’re still given for certain tough infections, sometimes even for things like respiratory infections when they shouldn’t be. Overuse or unnecessary use of these drugs can rapidly damage your kidneys, sometimes irreversibly. If you’re ever prescribed one, it’s worth asking your doctor, “Is this truly necessary, or is there a safer alternative?”
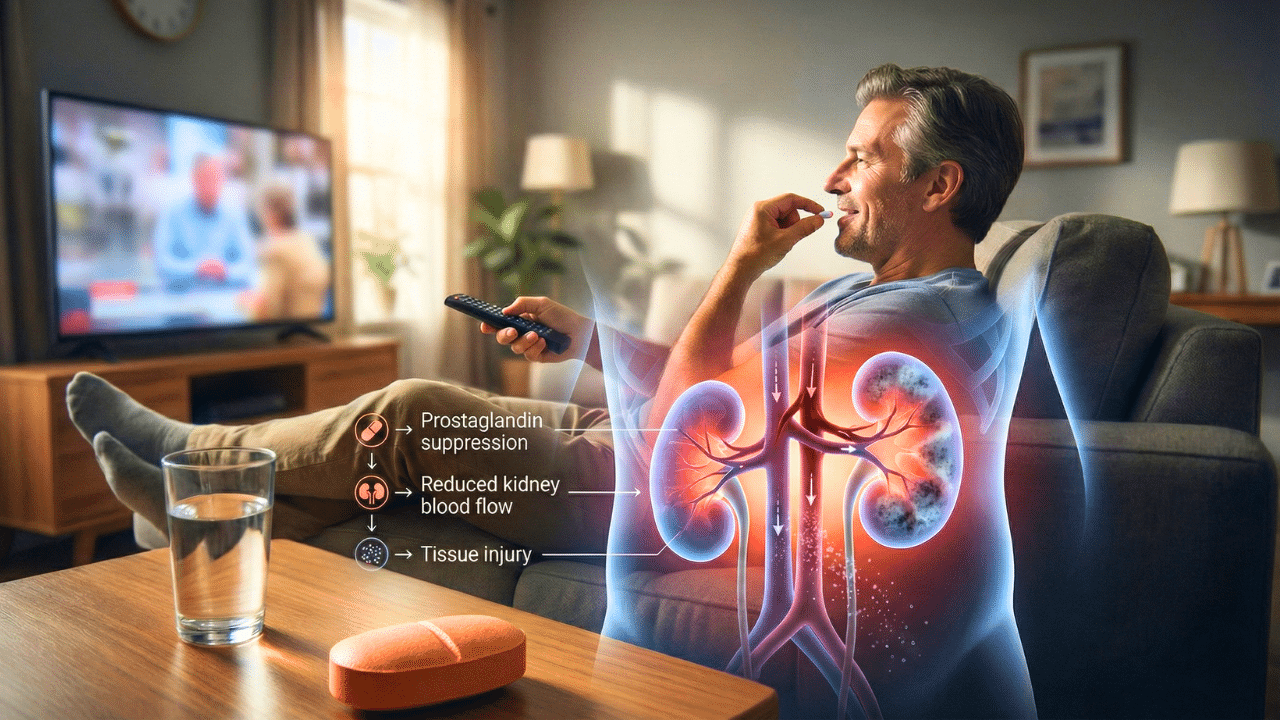
2. Pain Relievers: Ketorolac, Ibuprofen, and Naproxen
These well-known, over-the-counter medications are everywhere. While taking them occasionally for short-term pain is generally safe for most people, the trouble arises when they’re used daily or for chronic pain. Frequent use can lead to chronic kidney disease because these drugs reduce blood flow within the kidneys. If you’ve got ongoing pain, it’s wise to discuss with your healthcare provider about alternatives with less risk to your kidneys.
3. ACE Inhibitors and ARBs (like Captopril, Enalapril, Lisinopril, and Telmisartan)
These are blood pressure medications commonly prescribed for people with hypertension, diabetes, or heart problems. Used the right way, they can actually be kidney-friendly—especially when blood pressure is well controlled. But, in certain situations—like if you already have rapidly declining kidney function—they can push a delicate kidney over the edge. Managing these drugs absolutely requires regular monitoring and check-ins with your doctor.
4. Statins (Atorvastatin, Pravastatin, Simvastatin)
Statins are used to lower cholesterol and protect your heart. For most, they’re very helpful and safe, but in some cases, particularly if you already have kidney issues or other risk factors, these can add extra stress to your kidneys. If you’re recovering from major heart surgery or recently had stents put in, the benefit often outweighs the risk, but always ask your doctor if the medicine is still right for you as your health changes.
5. Metformin
This drug is the first-line treatment for type 2 diabetes and usually works well for many people. However, after years of use, metformin can sometimes start to stress the kidneys—especially in those with declining kidney function. Most people won’t run into serious trouble after a short course, but if your kidneys are already fragile, it’s something your doctor needs to watch for.
6. Proton Pump Inhibitors (PPIs) like Omeprazole, Esomeprazole, Lansoprazole
If you take medicine for acid reflux or heartburn, you might be on a PPI. These drugs can be lifesavers for acid-related stomach issues, but using them long-term has been linked to chronic kidney disease for some people. If you’ve been on them for months or years, it’s a good idea to ask if you still need them, or if there are safer alternatives.
7. The Role of Supplements and Over-the-Counter Substances
It’s not just prescription drugs—some supplements and even certain “natural” remedies or liquid medicines can damage your kidneys, too. Because these products are less strictly regulated, you may not always know what’s in them. Some may interact with prescribed medications in harmful ways. Always keep your healthcare provider in the loop about anything you’re taking—even vitamins!
How Do You Know If Your Kidneys Are in Trouble?
Kidney disease often sneaks up without big warning signs. But there are clues:
- Blood tests showing rising creatinine or urea levels
- Bloodwork showing high potassium, low magnesium, or other chemical imbalances
- Swelling in your legs, puffiness around your eyes, or foamy urine
- Decreasing urine output (if you’re well-hydrated)
If you see these in your lab results, or just aren’t sure how your kidneys are doing, ask your doctor: “How are my kidneys doing? Should we run a kidney function test or see a specialist?”
The Good News: Many Kidney Injuries Are Reversible
For a long time, doctors thought kidney damage couldn’t be undone. But today, we know that many cases—especially those caught early—can see great improvement. Sometimes, just switching or stopping a single medication can help your kidneys recover function, sometimes dramatically. For chronic, long-standing kidney disease, goal number one is slowing progression by catching and fixing problems early.
What YOU Can Do to Protect Your Kidneys
- Control blood sugar and blood pressure—preferably with diet and lifestyle, not just with medications.
- Have your kidney function checked regularly, especially if you’re on several meds.
- Ask about every prescription: ‘Is it safe for my kidneys?’ or ‘Is there a safer alternative?’
- For pain or acid reflux, ask if you can come off medication or switch to something less harmful if you’ve been taking it long term.
- Let your doctor know about any supplements or over-the-counter drugs you’re using.
In Conclusion
Medications are sometimes necessary for your health, but some can do more harm than good when it comes to your kidneys—especially with long-term use. The earlier you and your doctor identify possible risks, the better chance you have to keep your kidneys healthy for years to come. The key is awareness, proactive conversations, and regular monitoring. Don’t wait for a problem to show up—take steps to protect your kidneys today!
If you have concerns or are experiencing symptoms, always consult with your healthcare provider before making any changes to your medication regimen.
Source: Dr. Antonio Cota

