Are you or a loved one taking gabapentin (Neurontin)? This medication is everywhere—prescribed for nerve pain, seizures, and much more. But what if this “helpful” drug is hiding a threat to your mind? Today, we’re diving deep into some alarming new research: gabapentin may actually increase the risk of cognitive decline and dementia, especially in older adults. Before you reach for your next dose, let’s uncover the truth together. (Based on the insights of Dr. Suneel Dhand)
Key Takeaways
- Chronic use of gabapentin is linked to a higher risk of cognitive impairment and dementia.
- Elderly patients seem especially vulnerable to gabapentin’s sedative and mind-dulling effects.
- Overprescribing and increasing dosages may make matters worse over time.
- Many people don’t realize their mental fog or drowsiness could be medication-related.
- Polypharmacy (taking many meds) adds to the confusion and risk for older adults.
- While gabapentin can be necessary for some, it’s not as safe as it’s often made out to be.
- Talk with your healthcare provider before making any medication changes, but always stay informed!
1. Gabapentin Is Not as Benign as Many Believe
Gabapentin has become a staple in prescriptions for nerve-related pain, seizures, and even conditions like shingles. While it seems like a wonder drug for some, the truth is that gabapentin is powerfully sedative. Many people—especially the elderly—receive this medication in massive, escalating doses because they develop tolerance over time. This means the more you take, the less effective it gets, prompting doctors to increase the dose, sometimes to unsafe levels. This cycle can leave patients chronically sedated, groggy, and at risk for more serious cognitive effects.
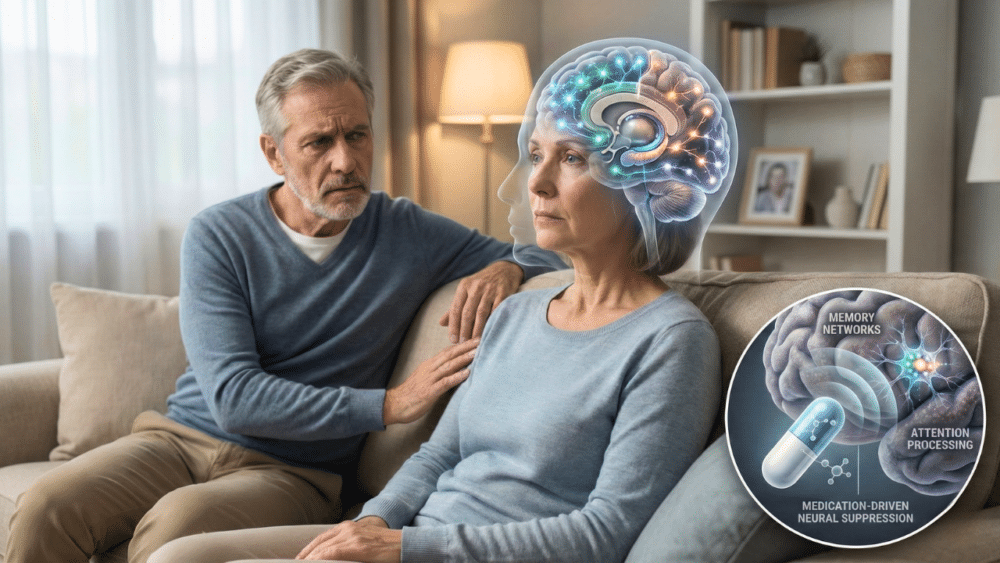
2. Alarming Studies Link Gabapentin to Cognitive Decline

In a recent study, researchers examined more than 26,000 adults (many suffering from chronic pain, like back pain) over a ten-year era. They found that people with six or more gabapentin prescriptions had an 85% higher chance of being diagnosed with mild cognitive impairment compared to non-users. Even more troubling, these users also showed a 29% higher chance of developing dementia, according to medical publications. While these numbers are shocking, what’s especially concerning is how often these risks aren’t discussed with patients upfront.
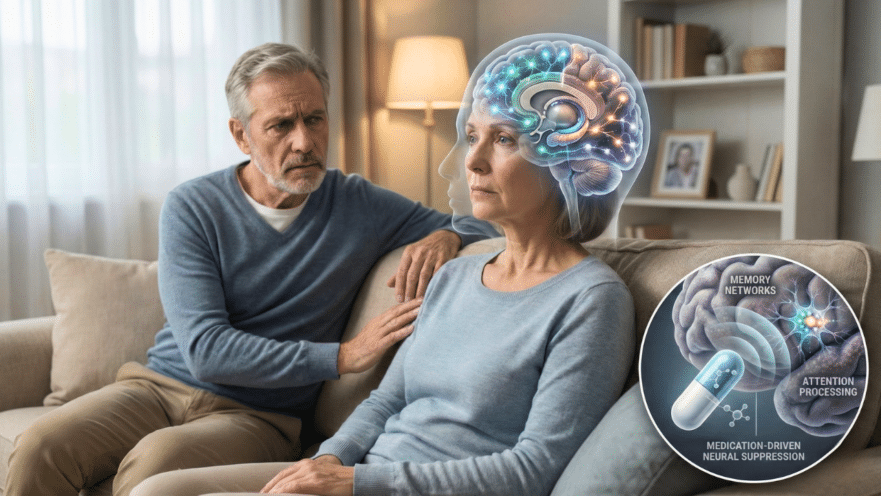
3. Elderly Patients Are Especially at Risk
If you’re over 65, the odds are stacked even higher. Medical doctors have noted that older adults on high doses of gabapentin often appear drowsy, confused, or mentally dulled—sometimes to the point that family members don’t recognize their normally alert loved ones. Once the medication is reduced or stopped, people often “wake up” and return to their more usual selves. For any family evaluating unexplained mental changes in a loved one, a medication review should always be on the checklist.
4. Overprescribing and Polypharmacy Worsen the Problem
Over 50% of people over age 70 are on at least five prescription medications—and often, the older you get, the more you take. Add a drug like gabapentin (known for drowsiness and cognitive side effects) to the mix, and you have a recipe for disaster. Mix-ups, medication interactions, and cumulative sedative effects can easily tip someone into confusion, falls, and serious long-term decline. Doctors are increasingly concerned that the trend of “more prescriptions for more problems” is hurting, not helping, our seniors.
5. Cognitive Side Effects Often Go Unnoticed
It’s shockingly common for people on gabapentin to gradually become more sluggish, forgetful, or less engaged—and not realize their medication may be to blame. Many families attribute these changes to “getting older” or dementia, when sometimes, reducing a sedating medication like gabapentin leads to rapid improvement. Always be on the lookout for mental changes linked to new or increased prescription drugs, and ask your doctor about alternatives if you notice a difference.
6. The Science Has Its Limits—but the Warning Signs Are Real
While the major study on gabapentin and dementia was well-constructed, it wasn’t perfect (no study is). It followed people in a real-world setting, without tracking every pre-existing condition or medication they were taking. This means the causative relationship isn’t conclusively proven—but the large increase in cognitive risks lines up with what many doctors have observed in practice. If a medication is making you drowsy or foggy, it stands to reason it could have long-term impacts on your mental fitness as well.
7. It’s Time to Re-Think Our “Pill for Every Problem” Mentality
Doctors and patients alike have been swept up in a culture where every symptom must have a pill. For pain, for sleep, for mood—gabapentin is often viewed as a quick fix. But every medicine comes with tradeoffs, and for gabapentin, those may include real cognitive costs. The antidote? Awareness, open conversation, and a focus on non-pharmaceutical solutions whenever possible. Physical therapy, lifestyle changes, and integrative approaches often make a bigger difference over time, with fewer risks to the mind and body.
Conclusion: Your Brain Is Worth Protecting!
When it comes to medications like gabapentin, the risks deserve as much attention as the potential benefits. Whether you take gabapentin yourself or care for someone who does, be proactive. Ask your healthcare provider about cognitive changes, possible alternatives, and the real risks of long-term use. Your brain—like the rest of your health—is worth protecting.
Source: Dr. Suneel Dhand