Are you worried about your kidney health or looking for ways to protect and support your kidneys? What if I told you that certain supplements, when used correctly, could potentially slow the progression of kidney disease by up to 25%—and this isn’t just wishful thinking, but scientific fact? If that caught your attention, you’re in the right place!
If you or a loved one are dealing with chronic kidney disease (CKD), you know that treatment can feel overwhelming. With so much conflicting information out there, how do you sort out which supplements are truly helpful, and which are just hype? Today, let’s break down the most promising, medically backed supplements for kidney disease. I’ll explain how they work, what the research actually says, and what questions to ask your doctor about before getting started. Let’s dive in! (Based on the insights of nephrologist Dr. Sean Hashmi)
Key Takeaways
- The right supplements can support kidney health but should never replace medical treatments or a healthy lifestyle.
- Vitamin B and D, omega-3 fatty acids, specific probiotics, niacin, keto analogues, calcium citrate, inulin, antioxidants, and even creatine have strong evidence for certain CKD populations.
- Always consult your nephrologist before adding new supplements.
- Supplements should address your specific deficiencies and disease stage, with regular lab monitoring.
1. Water-Soluble Vitamins: Essential for Energy and Red Blood Cells
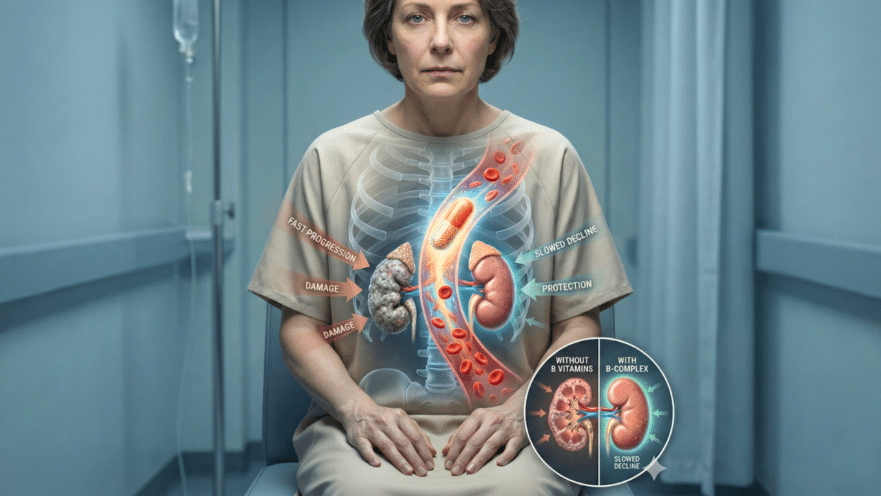
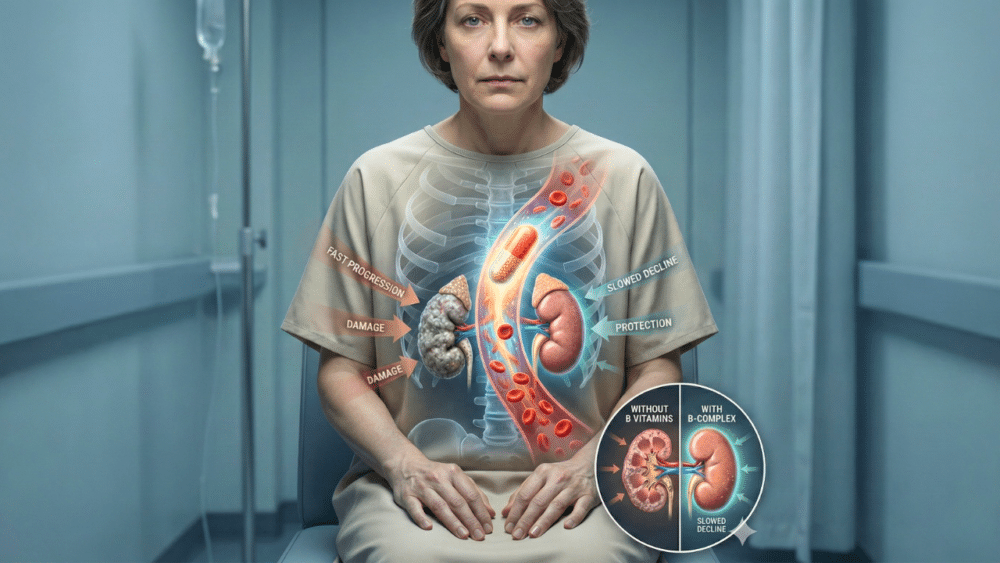
Kidney disease, especially in advanced stages or during dialysis, often strips your body of vital water-soluble vitamins like the B-complex group (B1, B2, B6, B12, and folate) and vitamin C. These nutrients are crucial for maintaining energy, healthy nerves, and blood cell production—areas frequently impacted by CKD.
According to medical guidelines, 30-50% of people with chronic kidney disease are low in B vitamins, and supplementation is recommended for stages 4 and 5. Moderate vitamin C can also help lessen the need for anemia medication in dialysis; just don’t overdo it, as high doses can lead to kidney stones.
Pro tip: Regularly check your B vitamin levels. If you’re deficient, supplementation under your doctor’s supervision may help improve how you feel and function.
2. Vitamin D: The Overlooked Protector of Bones and Immune Health
Vitamin D isn’t just a “bone vitamin.” In CKD, your body struggles to activate vitamin D, leading to weak bones and increased parathyroid hormone levels. Supplementing with over-the-counter D2 or D3 can boost your vitamin D status by 30-50% and lower parathyroid hormone by up to 40%, lowering the risk of fractures by 15-20%.
Recent research also points to immune and anti-inflammatory benefits, possibly slowing kidney damage. Talk to your nephrologist about checking and correcting vitamin D levels—this is a supplement with benefits that go way beyond your skeleton.
3. Omega-3 Fatty Acids: For Heart and Kidney Protection
If you think omega-3s from fish oil or algae are only for heart health, think again. A 2021 review showed dramatic improvements: total cholesterol dropped by about 26%, triglycerides by 22%, and cell-damaging molecules (oxidative stress markers) by an impressive 91%.
Omega-3s act on blood vessels, not only cooling inflammation but also repairing the delicate lining. For CKD patients, that means less heart risk (a major killer in kidney disease) and possibly slowed CKD progression. Choose pharmaceutical-grade omega-3s—these are purified for best results.
4. Probiotics and Prebiotics: The Gut-Kidney Connection
Did you know your gut bacteria can speed up or slow down kidney damage? Certain “good” probiotics—like Lactobacillus acidophilus, Lactobacillus casei, Bifidobacterium lactis, Bifidobacterium longum, and Streptococcus thermophilus—have been shown to slash kidney-harming toxins by up to 30% and even modestly improve kidney filtration.
Prebiotics like inulin (a type of fiber) serve as fuel for these beneficial bacteria, further reducing kidney toxins and helping mineral absorption. Together, they can lower inflammation markers by as much as 75% in some studies. Consider a high-quality probiotic alongside inulin-rich foods or supplements for maximum benefit.
5. Niacin: A Powerful Ally for Managing Phosphates
High phosphorus is a silent threat in CKD, causing blood vessel damage and heart attacks. While most treatments bind phosphate in the gut, niacin works differently—it blocks the absorption of phosphate in your intestines and kidneys. Clinical studies show that niacin supplements can lower blood phosphate by 20–30%, especially beneficial in stage 3B and beyond. Start slow to avoid the “niacin flush,” and always work closely with your doctor.
6. Keto Analogues: Preserving Muscle and Reducing Waste
Keto analogues of amino acids offer a cutting-edge approach to support people on low-protein diets. These provide the essential building blocks for your body minus the nitrogen waste that stresses the kidneys. Research shows keto analogues help preserve muscle mass by 15–20%, cut uremic symptoms by up to 40%, and can delay dialysis by several months. If you’re on a low-protein diet, ask your dietitian about adding keto analogues.
7. Calcium Citrate and Inulin: Smarter Mineral Management
The type of calcium supplement you take actually matters! Calcium citrate is better absorbed (even with reduced stomach acid), causes fewer digestive side effects, and lowers the risk of kidney stones by up to 50% compared to other forms. If you need calcium supplementation for bone health, bring this up with your doctor.
Inulin, as discussed above, is a prebiotic fiber that can enhance mineral absorption and reduce harmful toxins. It’s a kidney-friendly choice that supports your gut health, too.
8. Antioxidants: Defending Your Kidneys from Oxidative Stress
Kidney disease puts your cells under constant fire from free radicals—unstable molecules that accelerate kidney damage. Antioxidant supplements can offer extra protection, much like applying “rust proofing” to your kidneys:
- Alpha lipoic acid: Bolsters cell antioxidants, with research showing a 30-50% rise in protective capacity.
- Coenzyme Q10 (CoQ10): Supports energy production and reduces vascular stress.
- N-acetylcysteine (NAC): Precursor to glutathione, helps lower inflammation and protein in urine.
- Acetyl-L-carnitine and turmeric (curcumin): May further reduce fatigue and inflammation.
All of these have shown promising results for managing oxidative stress in CKD, though more studies are needed. Always discuss dosing and timing with your medical team.
9. Creatine: A Surprising Emerging Supplement for Dialysis Patients
Creatine has long been shunned in people with kidney issues, but new studies, especially in dialysis patients, are changing the conversation. Research from 2024 shows creatine supplementation can increase muscle mass, reduce inflammation, and even cut muscle cramps by 60%—a common source of misery on dialysis.
As kidney function drops, your body’s ability to make creatine naturally declines. This can lead to muscle wasting, fatigue, and even brain fog. For dialysis patients struggling with cramping or frailty, discuss this option with your nephrologist—it’s a promising new avenue, though still considered experimental in most settings.
Putting It All Together: Supplement Tips for Kidney Health
- Always consult your nephrologist before starting any new supplement.
- Test for deficiencies (especially vitamin D and B vitamins) and tailor your approach.
- Focus on quality over quantity; high-evidence supplements like B vitamins, vitamin D, and omega-3s are a good place to start.
- Track your kidney stage: The right supplement for a stage 3 patient may differ from someone on dialysis.
- Monitor regularly with labs to adjust as needed and catch any medication interactions early.
- Remember: Supplements are part of, not a replacement for, medical care and dietary guidance!
Final Thoughts
In summary, evidence supports several key supplements—including water-soluble vitamins, vitamin D, omega-3s, niacin, keto analogues, probiotics, calcium citrate, inulin, antioxidants, and even creatine for select patients—can help slow kidney disease progression and improve quality of life. However, everyone’s needs are unique, and a cookie-cutter approach can do more harm than good.
The main takeaway? Partner closely with your healthcare team. Stay informed, advocate for testing, and prioritize supplement choices with real science behind them. By combining careful supplementation with diet, medication, and lifestyle, you can give your kidneys their best fighting chance.
Source: Dr. Sean Hashmi