
Do you come home at the end of a long day and feel like you’re dragging around heavy, achy, swollen legs? Is the skin around your ankles starting to look thick, reddish, or discolored? This might be more than just typical end-of-day swelling. It could be a condition called lymphedema.
I’m going to break down everything you need to know about lymphedema—what it is, what causes it, and most importantly, the practical, effective treatments you can start using to manage it. We’ll cover the tricks of the trade, from simple home remedies to the best gear you can get to find relief. While the word “lymphedema” can sound intimidating, and you may have even heard there’s no cure, I want to give you hope. There is a tremendous amount you can do to improve your quality of life, reduce the swelling, and protect your health. We’re going to cover it all, right now. (This article draws upon the knowledge of Dr. Tom Biernacki)
Key Takeaways
- Know Your Swelling: Lymphedema is different from regular edema. It involves protein buildup that can cause thick, hard, and discolored skin, increasing health risks like infections.
- Medical Diagnosis is Non-Negotiable: Before starting any treatment, see your doctor to rule out serious underlying conditions like heart, kidney, or lung problems.
- Compression is Crucial: Using compression socks, wraps, and sequential compression devices is one of the most effective ways to manage fluid buildup in your legs.
- Skin Care is a Priority: You must address the thick, dry, scaly skin associated with lymphedema through soaks, special wraps, and consistent moisturizing to prevent complications.
- Movement is Medicine: Regular exercise, stretching, and improving your flexibility can dramatically improve circulation and reduce swelling by making your muscles work more efficiently.
- Support Your Foundation: The right footwear, including supportive slippers and shoes with orthotics, can reduce the strain on your leg muscles, leading to less swelling.
7. First, Understand the Difference: Lymphedema vs. “Normal” Swelling
Many people experience swollen feet and ankles after a long day of work, especially if they stand or sit for hours. This is often a condition called venous stasis edema. It’s uncomfortable, for sure, but lymphedema is a more serious issue. With lymphedema, your lymphatic vessels—the system responsible for draining fluid and waste from your tissues—are damaged. They can’t do their job properly.
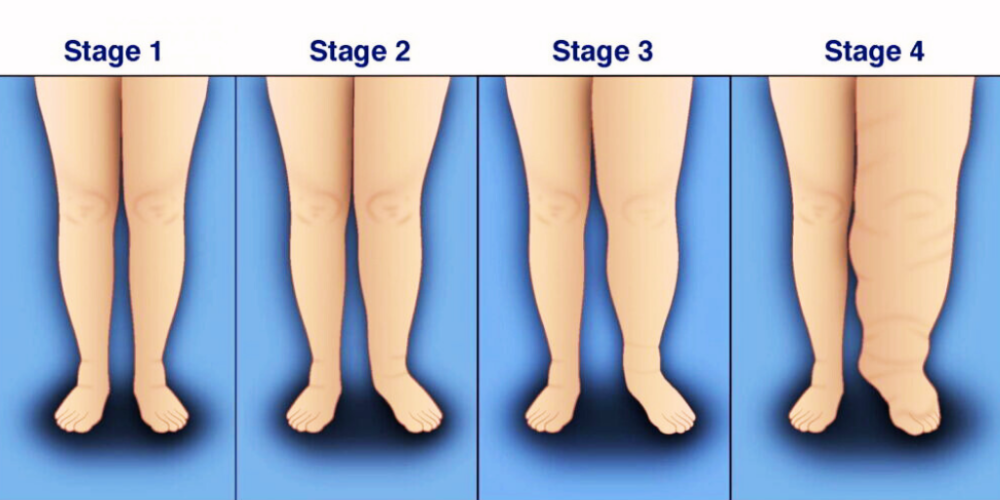
This means that not only does fluid accumulate, but protein also gets trapped in the tissues, typically in gravity-affected areas like your ankles and feet. This protein buildup is what causes the hallmark signs of lymphedema: the skin starts to turn hard, thick, and scaly. You might notice a reddish or brownish discoloration. In severe cases, it can resemble a condition called elephantiasis, with the skin taking on a tree-bark-like texture. This isn’t just a cosmetic problem; this poor skin quality dramatically increases your risk of dangerous infections like cellulitis. It’s a vicious cycle that can stop you from exercising and moving, making the condition even worse. Often, what I see in my patients is a combination of both venous stasis and lymphedema, but once you see that thick, indurated skin, you know you’re dealing with a lymphatic component.
6. Why You Absolutely Must See a Doctor First

Before you try any of the solutions we’re about to discuss, your first step must be to get a proper evaluation from a medical professional, like your internal medicine doctor or a podiatrist. Swelling in the legs can be a symptom of very serious underlying diseases, including congestive heart failure, kidney problems, or lung issues. These conditions are essential to diagnose and treat first.
Your doctor will perform a thorough history and physical exam and may order tests like X-rays, MRIs, lab work, or other scans. If you have a heart problem, you need to see a cardiologist. If it’s a kidney issue, a nephrologist. If you have diabetes, an endocrinologist. Treating the root systemic disease is paramount. This guide is coming from my perspective as a podiatrist, focusing on what we can do for your feet and legs directly, but it is not a substitute for a comprehensive medical workup.
5. The Power of Compression: From Socks to Machines

Compression is one of the cornerstones of managing lymphedema and venous stasis. The goal is to mechanically squeeze the fluid out of your tissues and back into circulation. There are a few great ways to do this.
- Compression Stockings: These are a fantastic tool for daily management. However, many people make a mistake here. Your doctor can prescribe very high-strength compression socks (e.g., 30-40 mmHg), and insurance might even cover them. The problem? They are incredibly tight and difficult to put on. In my experience, 98% of patients who get them simply don’t wear them. My advice is to start with a lower compression level, like 15-20 mmHg. You can buy these online for a very low cost—sometimes just a couple of dollars per pair. Get used to wearing them. See how they fit into your routine. If you feel they’re helping but you need more, then you can consider moving up to a higher strength. Don’t waste time and money jumping through hoops for a prescription-strength sock you’ll hate wearing.
- Sequential Compression Devices: These are inflatable cuffs that wrap around your calves or entire legs and rhythmically squeeze and release, pushing fluid up and out. For true, severe lymphedema, a doctor can prescribe a medical-grade device. But for many people with a mix of lymphedema and venous stasis, you can buy excellent consumer versions online for around $50-$100. I personally use one while working at my computer. It makes a huge difference in energy levels and prevents that end-of-day achiness and swelling. When you use one, start on the lowest setting, as they can be quite powerful. Using it for an hour or two while you watch TV can remove pounds of fluid weight from your legs.

