Did you know that every year, diverticulitis leads to over 300,000 hospital admissions in the United States alone? What’s even more alarming is that this number is climbing annually. For many, the first time they even hear the word “diverticulitis” is when they are already in the emergency room, dealing with intense pain and a serious medical situation. This doesn’t have to be your story. Your body often sends out warning signals long before a crisis hits, but these signs can be subtle, confusing, or show up in places you’d never expect.
I’m here to walk you through seven specific warning signs of diverticulitis that could help you catch this condition early, potentially before it becomes a medical emergency or, for many of you, before it happens again. Some of these symptoms are so nuanced that they are occasionally missed by healthcare professionals, while others are so unusual that you might never think to connect them to your gut health. By understanding these signs, you can become a better advocate for your own health, ask the right questions, and get the care you need sooner. Let’s dive into what you need to be watching for. (Based on the insights of Joe Leech (MSc))
Key Takeaways
- Localized Pain is Key: The most common sign is a steady, sharp pain in the lower-left part of your abdomen, where the sigmoid colon is located.
- Infection Signals: A fever, sometimes accompanied by night sweats and localized heat over the abdomen, is a classic sign of the infection associated with diverticulitis.
- Confusing Bowel Habits: Sudden and unusual changes in your bowel movements, such as alternating between diarrhea and constipation, are a significant red flag.
- Urinary Symptoms: Due to the colon’s proximity to the bladder, diverticulitis can mimic a UTI, causing painful urination, frequency, and urgency.
- Referred Pain: The inflammation can cause pain in seemingly unrelated areas like your groin, hip, thigh, or even trigger systemic responses like chest tightness and leg numbness.
- Age Matters: Symptoms can present differently depending on your age. Older adults may show systemic signs like fatigue, while younger patients often have a more aggressive form of the disease.
- Persistent Bloating: Severe, localized bloating and an inability to pass gas, especially when paired with other symptoms, should not be dismissed as a simple digestive upset.
1. Pain in the Lower-Left Quadrant
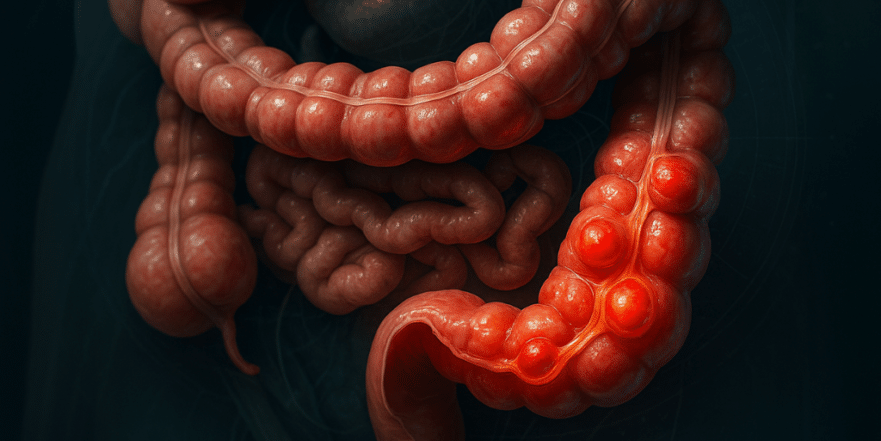
The first and most classic warning sign isn’t just abdominal pain—it’s the specific location of that pain. To understand why, you need to know a little about your anatomy. Diverticulitis occurs when small pouches, called diverticula, form in weakened spots along the wall of your large intestine (your colon). When these pouches become inflamed or infected, you have diverticulitis. These pouches most commonly develop in the sigmoid colon, which is the S-shaped final section of your large intestine located in the lower-left quadrant of your abdomen. Imagine drawing a plus sign with your belly button as the center; the lower-left square is where the action usually is.
This specific location is a crucial diagnostic clue. Pain in the other quadrants typically points to different issues. For instance, the upper-right quadrant houses your liver and gallbladder, so pain there might suggest gallbladder disease. The upper-left quadrant contains your stomach and spleen, and pain could be mistaken for an ulcer. The lower-right quadrant is home to your appendix, making pain there a classic sign of appendicitis. But that persistent, sharp, and steady pain locked into your lower-left side is the hallmark of diverticulitis. Unlike a stomach ache that might come and go, diverticulitis pain tends to set in, stay put, and gradually get worse. Interestingly, research has shown that in people of Asian descent, it’s more common for the diverticula to form on the right side, making it easy to confuse with appendicitis.
2. Fever and Night Sweats Most People Ignore
It’s essential to remember that diverticulitis is, at its core, an infection. When your body is fighting off an invader, its primary defense mechanism is to raise your internal temperature, resulting in a fever. This is your immune system going to war. However, the pattern of this fever can be very telling. Many people we’ve worked with describe not just a high temperature but also drenching night sweats. One person shared, “I get night sweats so bad I have to sleep on towels. My lower-left abdomen gets hot.” This combination of a fever, night sweats, and a feeling of localized heat over the painful area is your body’s inflammatory response in overdrive, directly targeting the infection in your colon.
That said, you can’t rely solely on the presence of a fever. Surprisingly, research indicates that about 15% of diverticulitis patients are “afebrile,” meaning they have no fever at all, or it’s just a very low-grade one. We’ve spoken with several patients who dismissed their slight fevers, thinking they were just feeling run down or fighting off a common cold. This is why it’s so important not to dismiss other symptoms just because you don’t have a high temperature. However, if you do have a fever, especially when it’s combined with that distinct lower-left abdominal pain, it’s a major warning sign that requires a same-day medical evaluation.
3. Bowel Changes That Seem Mixed and Confusing
When your colon is inflamed and infected, it’s no surprise that your bowel habits will be affected. But with diverticulitis, the changes can be particularly confusing and are often missed. You might experience diarrhea, constipation, or a strange mix of both. One patient described the progression this way: “It starts as a pain in the lower-left abdomen. Then the bowel movements start to change quickly, becoming less and less frequent.” They went on to describe a pattern of making multiple trips to the bathroom in the morning only to pass small, hard stools they called “rabbit pellets.” This is a classic sign of constipation where the colon is struggling to move waste along.
Another person described their experience as, “It’s bloating, cramps, little diarrhea alternating with brief constipation. Just all-around misery that happens out of nowhere.” This unpredictable swing between loose stools and blockage is a key indicator that something is wrong. The inflammation can irritate the colon lining, causing diarrhea, while the swelling can also create a partial blockage, leading to constipation. The most important thing for you to recognize is a sudden change from your normal pattern. If your bowel habits suddenly go haywire and this change is accompanied by abdominal pain, it’s time to consider that it could be more than just a simple digestive upset.
4. Urinary Symptoms That Fool Everyone (Including Doctors)
This next sign might surprise you, but diverticulitis can cause urinary symptoms that are frequently mistaken for a urinary tract infection (UTI). Here’s why: your sigmoid colon sits right next to your bladder. When the diverticular sacs in your colon become inflamed and swollen, they can physically press against the bladder. This pressure can irritate the bladder and lead to classic UTI-like symptoms, including painful urination, feeling like you have to go all the time (frequency), and a sudden, desperate need to urinate (urgency).
In more severe cases, a serious complication called a fistula can form. A fistula is an abnormal tunnel that connects the colon directly to the bladder. This allows gas and stool to pass from your intestine into your urinary system. One patient shared their harrowing experience: “I had none of the usual symptoms until the fistula had broken out and made my bowel join with my bladder. My first sign was air bubbles when I was urinating, and I experienced a burning feeling.” The key danger signs to watch for are pneumaturia (air bubbles in your urine), fecaluria (visible stool particles in your urine), and recurrent UTIs that don’t seem to clear up with antibiotics. If you’re experiencing urinary symptoms alongside abdominal pain, don’t just assume it’s a simple UTI, especially if you have a history of digestive issues.
5. Pain in Unexpected Places
It might sound strange, but the inflammation from diverticulitis can cause pain in parts of your body that seem completely unrelated to your gut. This is known as “referred pain,” where your brain misinterprets the pain signals coming from your inflamed colon and makes you feel the sensation elsewhere. One person described their experience like this: “I get what feels like pain in my groin, hip, or my upper thigh. As a teen, I used to get this when I had bad menstrual cramps.” This comparison is insightful because both conditions involve deep pelvic inflammation that can irritate the same nerve pathways.
The unusual symptoms don’t stop there. Another patient shared, “In a flare-up, my symptoms are cold hands and generally a panicky feeling with a tight chest. Also, my left leg feels numb—same side as the diverticulitis.” You might wonder how a colon problem could possibly cause chest tightness or a numb leg. This happens because significant inflammation triggers a systemic, body-wide response. Your nervous system can go on high alert, interpreting the inflammation in ways that can mimic anxiety symptoms or even heart problems. This is why diverticulitis is sometimes misdiagnosed as kidney stones, ovarian cysts, endometriosis, or even just severe menstrual cramps, particularly in women. The takeaway here is to pay attention when you have multiple, unexplained symptoms happening at once. Abdominal pain plus unusual sensations elsewhere could all be connected to that single inflammatory process in your gut.
6. Atypical Presentations in Different Age Groups
Diverticulitis does not present the same way in everyone, and age is a major factor. In older adults, the disease often shows up with systemic symptoms rather than the classic localized pain. An elderly patient might present with general fatigue, unexplained fainting episodes (syncope), or even acute kidney problems, with little to no complaint of abdominal pain. This makes diagnosis incredibly difficult. In fact, a 2025 study concluded that a CT scan should be strongly considered for any patient over 65 who is suspected of having diverticulitis but presents with these atypical, systemic signs.
On the other end of the spectrum, diverticulitis is becoming increasingly common in people under 50. However, these younger patients often face skepticism from doctors who may still view it as an “older person’s disease.” The concerning reality is that younger patients are twice as likely to be misdiagnosed, yet they often have a more aggressive form of the disease that more frequently requires surgery. Perhaps the most dangerous cases of all are those that don’t cause much pain. As one person noted, “The two times I had confirmed diverticulitis with a CT scan, I never had what I would consider lots of pain. I felt uncomfortable in my gut, but that’s it.” This illustrates that some cases manifest as a dull, persistent discomfort rather than severe, acute pain. This can lead people to delay seeking care, which is never a good idea when dealing with a potentially serious infection.
7. Persistent Bloating and Gas That Won’t Go Away
This final warning sign is one that many people are quick to write off, but it shouldn’t be overlooked. Persistent bloating and trapped gas are very common in diverticulitis, but they are often dismissed as symptoms of IBS or just “normal” digestive issues, which can delay a proper diagnosis. What makes this type of bloating different from the everyday variety is its pattern and severity. During a diverticulitis flare, patients often describe feeling like they are completely unable to pass gas. This inability to fart, combined with the swelling and inflammation in the colon, can create a partial blockage, leading to intense discomfort.
The bloating also tends to be more severe and localized. Many people report that their lower abdomen feels hard, distended, and tender to the touch, rather than the general, all-over bloated feeling you might get after a big meal. While bloating and gas are symptoms of many different digestive conditions, they become much more concerning when they are persistent, don’t respond to your usual remedies (like walking or over-the-counter gas relief), and are combined with the other warning signs we’ve discussed, such as left-sided pain, fever, or changes in bowel habits. The key is to recognize when your bloating isn’t just bloating anymore—it’s a signal that something more serious is happening.
Conclusion
Your body has a complex way of communicating with you, and learning to interpret its signals is one of the most powerful things you can do for your health. The symptoms of diverticulitis can be frightening and confusing, but understanding what’s happening inside your body empowers you to take the right action at the right time. If your symptoms don’t seem to add up, or if you feel like something is being missed, don’t hesitate to seek a thorough workup from your doctor. Never accept that it’s “probably just IBS” if you are experiencing multiple of these warning signs. By listening to your body and advocating for yourself, you can navigate your health journey with confidence and get the care you deserve.
Source: Joe Leech (MSc)