Have you ever found yourself worrying about what your blood pressure numbers should be? Maybe every time you visit your doctor, you hear about the mysterious “120 over 80” target. Is that number really ideal for everyone? Let’s dig deep into what blood pressure means and why finding your personal healthy range could be so much more important—and safer—than chasing a magic number. (Based on the insights of Dr. Suneel Dhand)
Key Takeaways
- Ideal blood pressure varies for each person—there is no one-size-fits-all answer.
- Target numbers like 120/80 are helpful guides, but not always appropriate for everyone, especially older adults.
- Overtreating blood pressure can cause dangerous side effects like dizziness and falls.
- Lifestyle changes, rather than more medications, are often the best way to manage blood pressure.
- Monitoring at home and working with your doctor is crucial for the most accurate picture.
1. Why You Have Two Blood Pressure Numbers
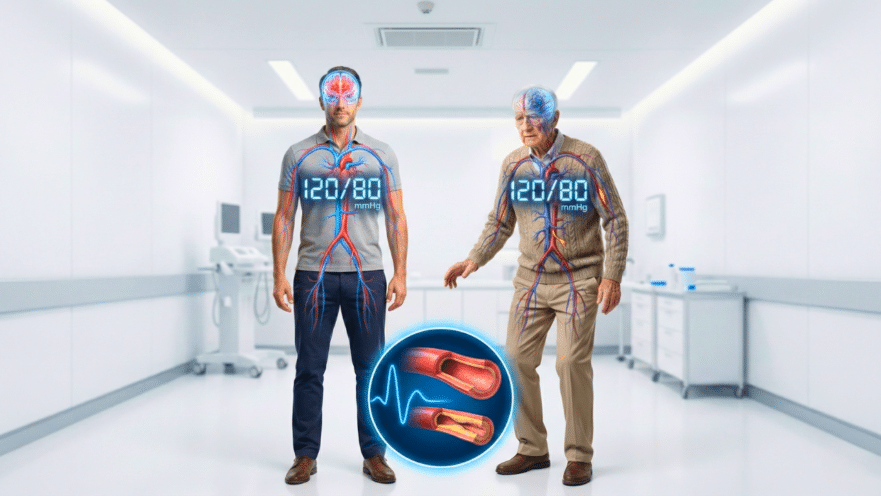
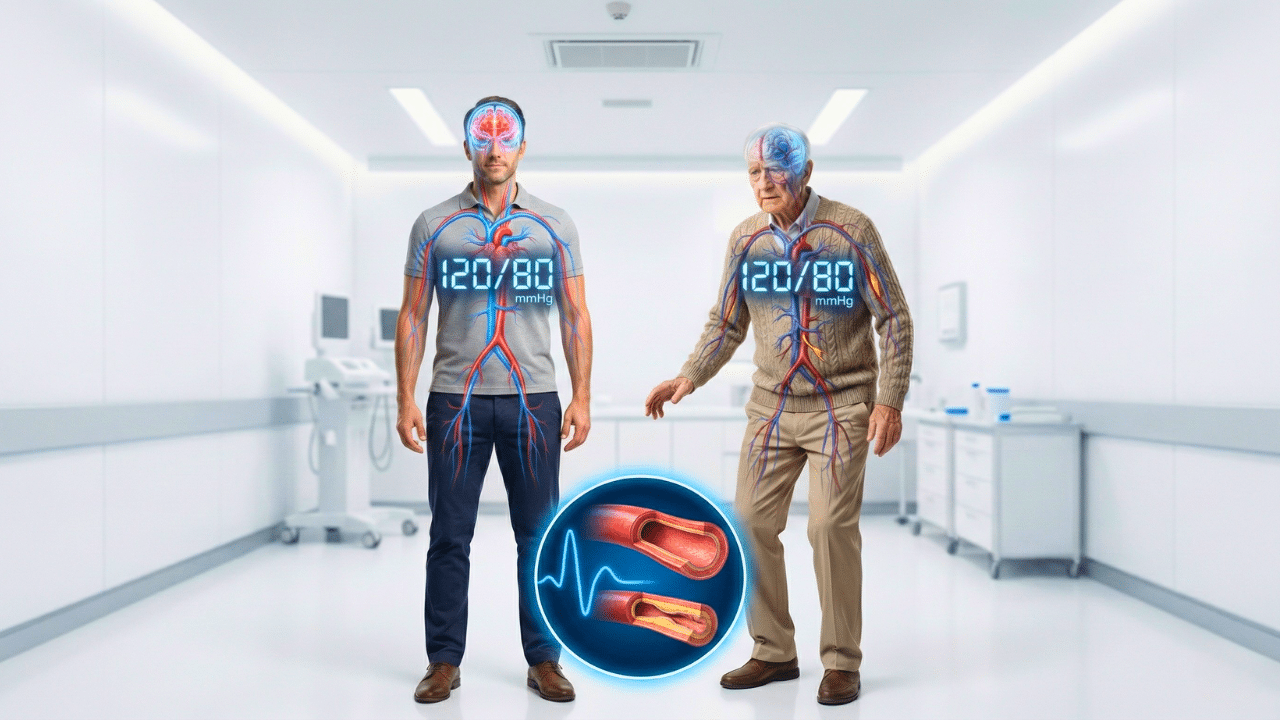
Your blood pressure reading has two numbers. The top number, called systolic, measures the force of blood when your heart contracts. The bottom number, diastolic, adds up the pressure when your heart relaxes. So, 120/80 means a systolic pressure of 120 mmHg and diastolic pressure of 80 mmHg.
2. Is 120/80 Really the Perfect Blood Pressure for Everyone?
Health authorities often cite 120/80 as the benchmark for healthy adults. However, doctors are beginning to push back against the idea that everyone—no matter your age, health status, or medication—is supposed to fit that mold. The truth? A number that works well for a 25-year-old might make an 80-year-old dizzy and weak.
3. Why Overly Strict Guidelines Can Cause Harm
Recent changes mean that even a blood pressure reading of 125/80 might be labeled as “elevated.” The problem is, if doctors strictly follow these guidelines without considering individual differences, people—especially seniors—end up overmedicated. This increases risks of fainting, weakness, and falls. Blanket guidelines can lead to unnecessary prescriptions and side effects.
4. One Size Does Not Fit All: Personalization Is Key
Doctors agree that the best blood pressure is often the safest—not always the lowest. Your ideal range should be set with your real-world circumstances in mind: age, activity, medical history, lifestyle, and how you actually feel. If lowering your numbers makes you feel dizzy or exhausted, it’s a strong signal that the plan needs tweaking.
5. Avoid Making Treatment Decisions on a Single Office Reading
Walking into your doctor’s office can make anyone nervous, and that anxiety (or just the stress of traffic) can artificially raise your numbers. Relying on one reading for medication decisions is risky. Home blood pressure monitoring over a period of two weeks, at different times of day, gives a much truer picture of your health.
6. Timing and Customization of Medications Matter
If you need blood pressure medications, timing can make a big difference. Taking all medications at once may cause sharp drops in blood pressure, especially in the morning. Doctors recommend splitting doses between morning and night for gentler, more effective results—and fewer side effects. The bottom line? Customizing your regimen with your doctor’s help is crucial.
7. The Hidden Danger of Overtreating Blood Pressure
Taking too many medications, or taking them the wrong way, can result in blood pressure dropping too low. If you (or a loved one) feel dizzy, especially when standing up, overly aggressive treatment might be the culprit. Signs to watch out for include weakness, brain fog, or increased fatigue, especially in older adults.
8. Why Lifestyle Changes Often Beat More Medication
Before adding new medications, it’s vital to assess lifestyle habits. Are you exercising regularly? Eating a balanced diet? Managing stress? Most cases of high blood pressure—especially in those under 60—are linked to insulin resistance and poor metabolic health, not just bad luck. Simple, consistent changes like eating less processed food and more whole foods, quitting smoking, and exercising can drastically improve blood pressure, sometimes within weeks.
9. Recognizing When Your Blood Pressure Really Needs Intervention
So, when is high blood pressure actually a problem? Symptoms like headaches, blurred vision, chest pain, or repeated readings above 150/90 (for most adults) warrant closer attention. However, numbers sometimes fluctuate and should be averaged over time. Consult your doctor, especially if you have other risk factors or symptoms, but don’t panic over a single high reading.
10. The Importance of Both Systolic and Diastolic Numbers
Both your top and bottom numbers matter. If they’re both elevated, or if there’s a large gap between them, it’s a sign your doctor needs to look deeper for underlying issues. In rare cases, unusual differences have their own health significance, and tailored care is needed.
11. Why You Should Trust How You Feel—Not Just the Numbers
If you feel great and your home readings are steady—even if they’re “slightly” above the perfect textbook number—it may be perfectly healthy for you. On the other hand, if medication is lowering your pressure and making you feel bad, that’s a red flag needing attention.
12. Metabolic Syndrome: The Real Culprit Behind Most High Blood Pressure
You’ve probably heard about how salt, stress, or genetics can raise your blood pressure. But did you know that insulin resistance—usually due to high sugar, processed food, and obesity—is the leading driver? By tackling your diet (think: less sugar and processed food), you not only help your blood pressure but also reduce your risk for a host of other diseases.
13. When to Be Concerned (and Take Action)
As a general rule, if your systolic (top) number is consistently creeping toward or over 150, or your diastolic (bottom) is in the 90s, it’s time to have a thorough discussion with your doctor. Symptoms, not just numbers, are crucial. Also, anyone who has irregular gaps between systolic and diastolic, or signs of organ strain, should get extra diagnostics like an echocardiogram.
14. Practical Tips to Take Charge of Your Blood Pressure
- Track your blood pressure at home using a validated device, at different times of day for 2 weeks.
- Record how you feel after medications—share this info with your doctor.
- Prioritize diet, exercise, stress reduction, and sleep for lasting blood pressure improvements.
- Partner with your doctor for a personalized treatment plan, rather than chasing a one-size-fits-all goal.
- Speak up if you notice new side effects after medication changes—your feedback is vital.
Conclusion: Trust Yourself and Work With Your Doctor
Ultimately, your ideal blood pressure is as unique as your fingerprint. 120/80 may be a good benchmark, but it’s not the golden rule for every person, especially as you age or manage other health issues. Personalized care, based on how you feel and multiple home readings, is essential. Remember—the safest blood pressure is the one that’s just right for you.
Source: Dr. Suneel Dhand