What if I told you that a nagging pain in your chest, one you might dismiss as indigestion or a pulled muscle, could be a silent warning of a heart attack? It’s a chilling thought, but 40% of people who have a heart attack die before even reaching the hospital. Many of them simply thought it was muscle pain or gas. This information could save your life or the life of someone you love. For over 20 years, I’ve seen too many cases of people who arrived at the hospital too late. The most tragic part is that many of them felt warning signs hours or even days before, but they ignored them, chalking it up to stress, fatigue, or heartburn. When they finally sought help, it was too late.
Today, I’m going to be direct with you and give you information that can literally mark the difference between life and death. In this article, you’re going to learn to recognize five different types of chest pain. You’ll know exactly when it’s an emergency and when it’s not, and I’ll give you a step-by-step action plan for each situation. But first, a crucial disclaimer: this article does not replace emergency medical attention. If you are experiencing chest pain right now, stop reading and call your local emergency number immediately. Don’t wait. Don’t hesitate. Just call. If you’re here to learn and be prepared, then pay close attention. (Based on the insights of Oswaldo Restrepo RSC)
Key Takeaways
- Classic Heart Attack: This is an absolute emergency characterized by intense, oppressive pressure in the chest that may radiate to the arm, jaw, or back, and is accompanied by symptoms like cold sweats, nausea, and shortness of breath.
- Unstable Angina: This is chest pain that occurs at rest or with minimal effort. It’s a critical warning sign that a heart attack may be imminent and requires urgent medical attention within hours.
- Non-Cardiac Pain: Many chest pains are not heart-related. Musculoskeletal pain is localized and changes with movement, while digestive pain often feels like burning and is related to meals. Anxiety can also mimic heart attack symptoms.
- Silent Heart Attacks: One in five heart attacks are “silent,” especially in people with diabetes, women, and older adults. Key warning signs are not chest pain, but rather extreme fatigue, unexplained shortness of breath, and persistent digestive discomfort.
- Prevention and Action: Knowing your cardiovascular risk factors (like high blood pressure, diabetes, and smoking) is crucial. Having a clear action plan for when chest pain strikes can save your life.
1. The Classic Heart Attack: An Absolute Emergency
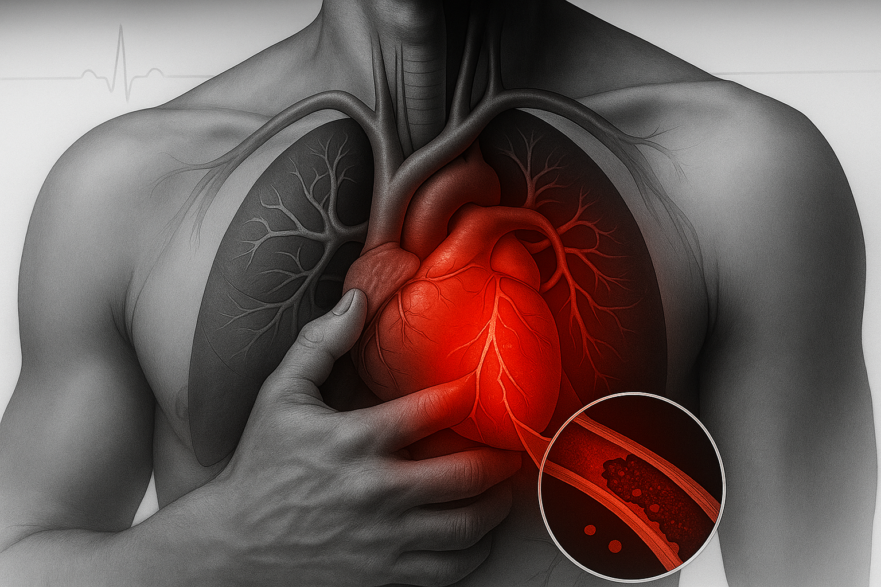
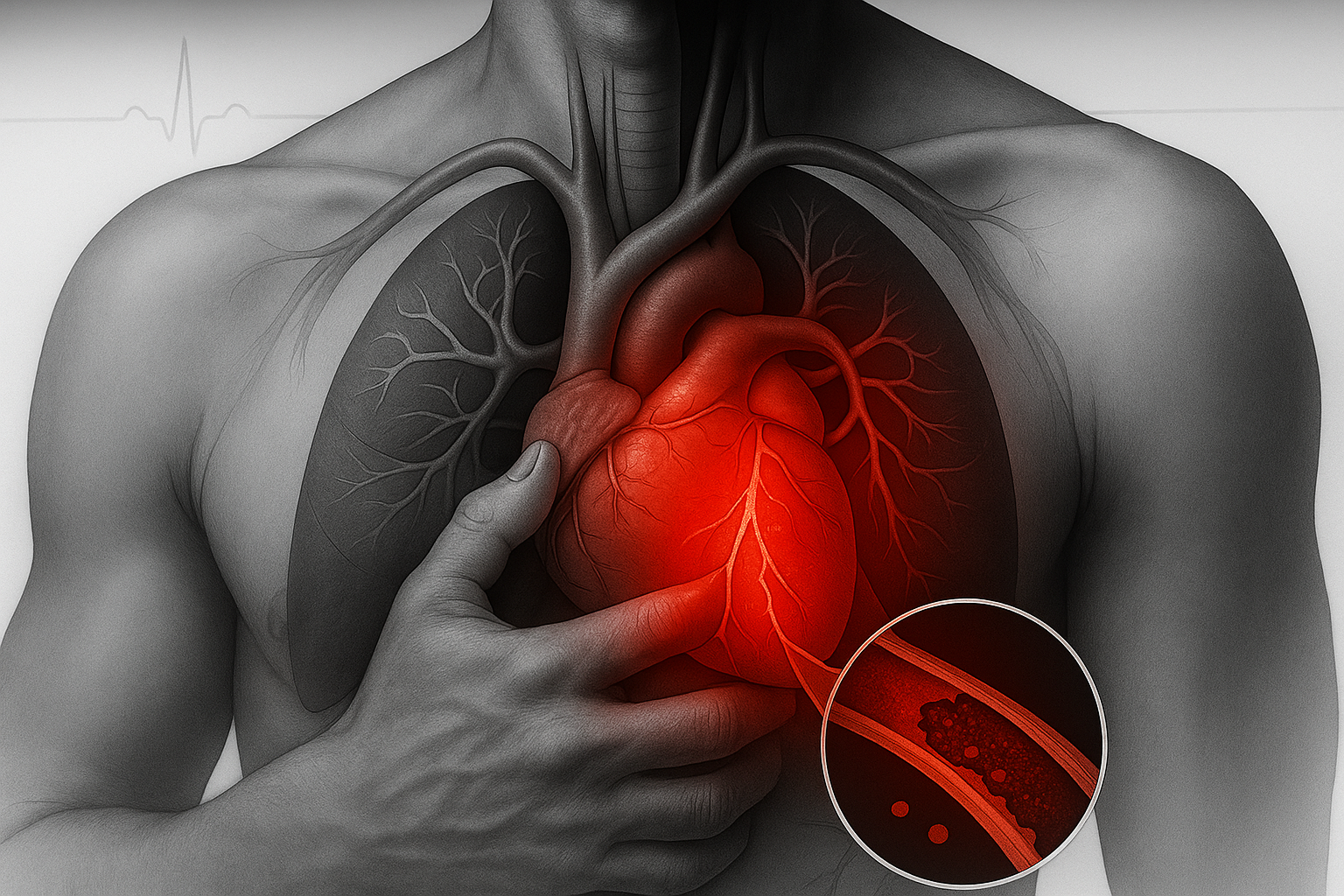
Let’s start with the most dangerous scenario: the classic heart attack. A heart attack, or myocardial infarction, happens when an artery supplying blood to your heart becomes completely blocked. Without blood, the heart muscle begins to die, and you have a very limited window to save it. The pain of a classic heart attack has very specific characteristics.
First, the location and sensation. The pain is typically felt in the center of the chest or slightly to the left. It’s not a sharp, stabbing pain like a needle. Instead, people describe it as an intense, oppressive, crushing pressure—as if a huge weight is sitting on your chest. This pressure is constant and doesn’t go away.
Second, the radiation. This pain doesn’t stay put. It travels, or radiates, to other parts of your body. Most commonly, it radiates down the left arm, particularly the inner part. It can also travel to your jaw, neck, back (especially between the shoulder blades), or even down into your stomach. Many people report their left arm feeling heavy, numb, or tingly.
Third, the accompanying symptoms. A heart attack rarely comes with just pain. It brings friends. Look for cold, clammy sweats (not from heat, but a chilling sweat), nausea or vomiting, and severe shortness of breath. You might feel dizzy, lightheaded, or like you’re about to faint. A very characteristic sign is a profound, irrational feeling of impending doom—a sense that something is terribly wrong.
Finally, the duration. Heart attack pain lasts for minutes, usually more than five, and sometimes 20-30 minutes. It is not relieved by rest, changing position, or taking deep breaths. If you have this type of pain, it is an absolute emergency. Call for an ambulance immediately. Do not attempt to drive yourself to the hospital.
2. Unstable Angina: The Ticking Time Bomb
The second type of dangerous chest pain is called unstable angina. Angina is chest pain caused by a lack of oxygen to the heart muscle because an artery is partially, not completely, blocked. There’s a critical distinction between stable and unstable angina.
Stable angina is predictable. It shows up when you exert yourself—climbing stairs, walking fast, carrying something heavy. You feel that pressure in your chest, you stop and rest for a few minutes, and the pain disappears. While not normal, it’s not an immediate emergency, but it does mean you need to see a cardiologist soon.
Unstable angina, however, is unpredictable and far more dangerous. It’s a sign that your heart is in imminent danger of a full-blown heart attack. The key signs of unstable angina are:
- Pain at rest: The chest pressure appears without any physical effort, while you’re just sitting, watching TV, or even sleeping.
- Pain with decreasing effort: You used to be able to climb two flights of stairs, but now you get chest pain after just half a flight.
- Pain that lasts longer: Your typical angina pain used to go away in two minutes, but now it lingers for 10, 12, or 15 minutes.
Unstable angina is a medical urgency. It’s not as immediately critical as an active heart attack, but it requires medical attention within hours, not days. Think of it as a ticking time bomb.
3. Musculoskeletal Pain: The Common Impostor
This is the most common type of chest pain and, thankfully, the least dangerous. This pain originates from the muscles, cartilage, or ribs in your chest wall—not your heart. The characteristics are very different from cardiac pain.
First, it’s a localized pain. You can often point with one finger to the exact spot that hurts, an area maybe the size of a coin. Cardiac pain is almost never like this; it’s a diffuse, widespread pressure across a larger area. Second, it changes with movement and pressure. If you twist your torso, change your position, or press on the sore spot with your finger, the pain gets worse. Cardiac pain does not change with movement or external pressure. Third, it changes with breathing. The pain intensifies when you take a deep breath and lessens with shallow breathing.
Finally, there’s often a clear cause, like you lifted something heavy, did an intense workout, or slept in an awkward position. And crucially, there are no accompanying symptoms like cold sweats, nausea, or shortness of breath. If your pain fits this description, it’s likely muscular. You can try a natural anti-inflammatory like turmeric or ginger, apply local heat, and rest. However, if you have cardiovascular risk factors, are over 50, or have diabetes or high blood pressure, don’t be too quick to self-diagnose. It’s always better to consult a doctor.
4. Digestive Pain: When Your Stomach Fools You
The fourth type of pain that can be confused with a heart attack is digestive pain. Your esophagus and stomach are located very close to your heart, and their nerve pathways are interconnected. This is why a digestive issue can feel exactly like a heart problem. The most common culprit is gastroesophageal reflux disease (GERD), where stomach acid flows back up into the esophagus, causing a burning sensation or pressure in the chest.
So, how can you tell the difference? Look at the timing: digestive pain usually appears after eating, especially after heavy, greasy, or spicy meals. Cardiac pain has no relationship with food. The sensation is also different: digestive pain is more of a burning, searing feeling that can rise into your throat, whereas cardiac pain is more of a pressure or weight. A key clue is relief with antacids. If you take an antacid and the pain improves within 5-10 minutes, it’s likely digestive.
Finally, position matters. Digestive pain often worsens when you lie down and improves when you sit up. The problem is, some heart attacks, especially those affecting the inferior (bottom) wall of the heart, can cause nausea and pain in the upper stomach, easily confused with indigestion. Therefore, if you have risk factors and the pain is intense, seek medical attention even if you think it’s digestive. It’s better to have a false alarm than to ignore a real heart attack.
5. Anxiety and Panic Attacks: The Mind-Body Connection
Finally, a panic or anxiety attack can produce very real, terrifying physical symptoms that perfectly mimic a heart attack. The pain from anxiety has a few distinguishing features. It often appears during moments of intense emotional stress. It’s frequently accompanied by hyperventilation (breathing very fast and deep), which can cause tingling in your hands and around your lips. Many people also experience a sense of unreality, as if they are outside their own body. The pain itself is often described as more sharp or stabbing rather than oppressive, and it tends to improve as you calm down. If you can sit down, practice slow, deep breathing, and focus on relaxing, the pain will likely diminish. Cardiac pain does not respond to relaxation techniques.
Here’s the challenge: the anxiety and the pain are real. Furthermore, some people have both anxiety and underlying heart conditions, and the stress of a panic attack can trigger a real cardiac event. For this reason, the very first time you experience these symptoms, you must get a medical evaluation, including an electrocardiogram (ECG), to rule out a heart problem. Once your heart has been cleared, you can then work on managing your anxiety with confidence.
The 3 Signs of a Silent Heart Attack
As promised, let’s uncover the signs of a silent heart attack. This is one of the most dangerous enemies because it doesn’t announce itself with obvious chest pain. As I mentioned, one in five heart attacks are silent or atypical, especially in three groups: people with diabetes (which can damage nerves that transmit pain), women (who often experience different symptoms than men), and older adults (whose nerve sensitivity may decrease with age). Here are the three signs to watch for:
- Extreme, Unexplained Fatigue: Suddenly, you feel utterly exhausted. This isn’t normal tiredness; it’s a profound exhaustion, as if you have no energy to even move. There’s no reason for it—you didn’t exercise, you slept well, but you’re drained. This fatigue can appear days or even weeks before the heart attack as your heart struggles to get enough oxygen.
- Shortness of Breath Without Cause: You suddenly find it hard to breathe while doing simple things that were easy before, like climbing a flight of stairs. Or you might wake up at night feeling like you’re suffocating. This happens because your heart isn’t pumping efficiently, causing fluid to back up in the lungs.
- Persistent Digestive Discomfort: This can manifest as frequent nausea, loss of appetite, a feeling of indigestion that won’t go away, or a mild ache in the upper abdomen. Many people, especially women, experience heart attacks that present primarily with these digestive symptoms.
If you have cardiovascular risk factors and experience any of these three signs, do not ignore them. See your doctor and ask for an ECG.
Conclusion: Your Heart Is Your Engine
Let’s quickly recap the most critical points. The classic heart attack involves intense chest pressure with radiation and other symptoms like sweating and nausea—a 911 emergency. Unstable angina is chest pain at rest and is an urgent warning sign. Silent heart attacks manifest as extreme fatigue, shortness of breath, or digestive issues. If you have risk factors, any chest pain should be taken seriously. But your best tool is prevention. Know your numbers (blood pressure, cholesterol, blood sugar), control your risk factors, and lead a healthy lifestyle. This information can save your life, but only if you act on it. Don’t wait for a heart attack to start caring for your heart. Start today. Your heart is irreplaceable. Protect it.
Source: Oswaldo Restrepo RSC