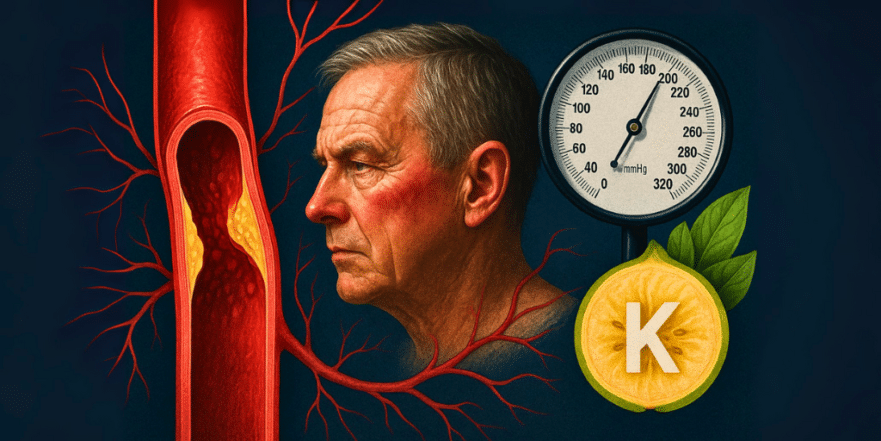
Did you know that a staggering 45% of adults in the US have high blood pressure? And if you’re over 60, that number jumps to a whopping 75%. That means three out of every four people in their later years will likely experience high blood pressure. Worldwide, over 1.3 billion people are affected. The big question is, why is this happening to so many of us as we age? The answer might be simpler than you think: a deficiency in one crucial nutrient – potassium.
This isn’t just about managing a number; it’s about understanding the root cause. Many common blood pressure medications work by targeting a system in your body called the Renin-Angiotensin-Aldosterone System (RAAS). But what if low potassium is what triggers this system in the first place? And what if increasing your potassium intake could be more effective than many of these medications?
Understanding How Your Kidneys Control Blood Pressure

Your kidneys play a vital role in regulating your blood pressure, and it all starts with a hormone called renin. When your kidneys release renin, it kicks off a chain reaction:
- Renin activates angiotensinogen: This inactive hormone, produced by your liver, gets converted into Angiotensin I.
- Angiotensin I becomes Angiotensin II: An enzyme then transforms Angiotensin I into Angiotensin II, the active molecule that really impacts your blood pressure.
- Angiotensin II constricts blood vessels: This narrowing of your blood vessels increases the pressure within them.
- Angiotensin II stimulates aldosterone: It also signals your adrenal glands to release aldosterone.
- Aldosterone tells kidneys to retain sodium: Aldosterone then instructs your kidneys to hold onto sodium, which in turn increases blood volume and further raises blood pressure.
This whole process, the RAAS, is designed to maintain blood volume. But when it’s constantly triggered, your blood pressure keeps climbing. This is where most blood pressure medications come into play. They are designed to interrupt this RAAS pathway at different points:
- Beta-blockers (like atenolol, metoprolol) reduce renin secretion.
- Direct renin inhibitors (like aliskiren) block renin directly.
- ACE inhibitors (like lisinopril, captopril) block the conversion of Angiotensin I to Angiotensin II.
- Angiotensin receptor blockers (ARBs) (like losartan, candesartan) block Angiotensin II from acting on blood vessels.
- Aldosterone blockers (like spironolactone) and diuretics (like thiazides, furosemide) work on downstream effects, like sodium retention.
Essentially, there are seven main classes of blood pressure medications, all trying to calm down this one system. But what if the system is being overactive because of a simple nutritional deficiency?
The Potassium Deficiency Connection

The trigger for this overactive RAAS system as we age is often a low intake of potassium. The average American consumes only about 2,300 mg of potassium daily, while experts recommend closer to 4,700 mg. For context, our hunter-gatherer ancestors likely consumed 8,000 to 10,000 mg of potassium daily.
Your kidneys have evolved over millions of years to use potassium as a gauge for your blood volume. With a diet rich in potassium, your kidneys understand you have adequate blood volume. But when potassium levels are low, your kidneys mistakenly think your blood volume is low. To compensate, they activate the RAAS, constricting blood vessels and retaining sodium, all in an effort to boost blood pressure and maintain that perceived low volume.
So, the problem isn’t necessarily a faulty system, but rather a lack of the signal (potassium) that tells the system to stand down. Low potassium levels are a direct signal to your kidneys to crank up the RAAS, leading to higher blood pressure.
Research Supports Potassium’s Role

What does the science say about replacing potassium? Multiple studies and meta-analyses have looked at the impact of potassium supplementation on hypertension. The results are quite compelling:
- Significant Blood Pressure Reduction: A meta-analysis of about 20 trials showed that potassium supplementation had a significant impact on reducing high blood pressure.
- Comparable to Medications: Another analysis of a dozen trials found that the blood pressure-lowering effect of potassium supplementation was comparable to many common medications that target the RAAS. Both typically show an average reduction of about 8 points in blood pressure.
By addressing the root cause – the potassium deficiency – you’re not just lowering your blood pressure; you’re potentially preventing the need for multiple medications. This approach can also reduce the risk of serious downstream health issues associated with high blood pressure, such as stroke, heart attack, and kidney failure.
Key Takeaways
- High blood pressure is incredibly common, especially as we age.
- The Renin-Angiotensin-Aldosterone System (RAAS) is a key regulator of blood pressure, controlled by hormones like renin and aldosterone.
- Most blood pressure medications work by interfering with the RAAS pathway.
- Low potassium intake is a major trigger for the RAAS system, leading to increased blood pressure.
- Our modern diets are typically very low in potassium compared to ancestral diets.
- Increasing potassium intake through diet or supplements can significantly lower blood pressure, often as effectively as medications.
- Addressing potassium deficiency tackles the root cause of hypertension, potentially reducing medication needs and associated health risks.
If you’re looking for a way to manage or even reverse high blood pressure without relying solely on medications, it’s worth exploring your potassium intake. Focusing on potassium-rich foods or considering supplementation could be a powerful step towards better blood pressure health.
Source: Dr. Dave Clayton